1. Understanding Obesity and Its Mechanisms
Obesity is defined as having an excessive amount of body fat, often measured by a body mass index (BMI) of 30 or higher. Obesity is a global health concern and is associated with a higher risk of developing numerous conditions, including heart disease, diabetes, and respiratory problems. In the case of a hiatal hernia, obesity plays a significant role in increasing the risk and severity of the condition.
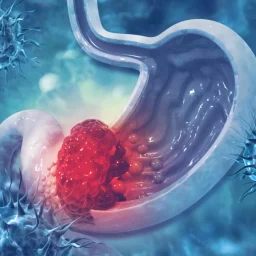
Increased Abdominal Pressure
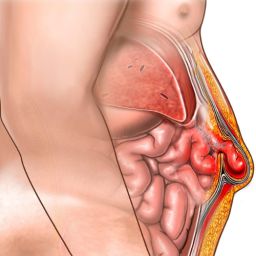
One of the primary ways in which obesity contributes to the development of a hiatal hernia is through increased abdominal pressure. When an individual has excess fat, particularly around the abdomen, it places extra pressure on the organs in the abdominal cavity, including the stomach. This increased intra-abdominal pressure can force the stomach upward, causing it to slide into the chest cavity through the diaphragm’s hiatus, leading to a hiatal hernia.
The pressure from excess abdominal fat is especially pronounced when an individual is sitting or lying down, as gravity and posture can further increase the chances of the stomach pushing upward into the chest.
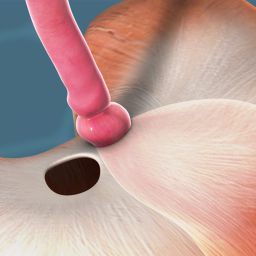
Weakened Diaphragm and LES

Obesity can also affect the diaphragm and the lower esophageal sphincter (LES), which work together to regulate the movement of food from the esophagus to the stomach. A weakened diaphragm, often associated with obesity, can no longer effectively support the stomach in its correct position. The LES, which acts as a barrier to prevent stomach acid from entering the esophagus, may also become weakened due to the increased pressure from abdominal fat. This leads to gastroesophageal reflux disease (GERD), a common condition associated with both hiatal hernias and obesity.
GERD is a major cause of acid reflux, heartburn, and regurgitation. The condition worsens in individuals with obesity, as the additional abdominal pressure makes it more difficult for the LES to function properly, allowing stomach acid to escape into the esophagus.
2. The Link Between Obesity and Hiatal Hernias
Studies have consistently shown a strong correlation between obesity and the development of a hiatal hernia. Individuals with higher body fat, especially abdominal fat, are more likely to develop a hiatal hernia due to the factors mentioned above. In fact, obesity has been identified as one of the most significant risk factors for the development of this condition.
Higher Prevalence in Obese Individuals
Several research studies have examined the prevalence of hiatal hernias among obese individuals. One study found that 60% of people with a BMI of 30 or higher had some form of hiatal hernia. This percentage increases significantly for individuals with a BMI greater than 35. Additionally, obesity has been found to be a significant factor in the severity of symptoms related to hiatal hernias, with obese individuals more likely to experience severe acid reflux, heartburn, and regurgitation.
Abdominal Obesity vs. Overall Obesity
Not all obesity is equal when it comes to hiatal hernias. Abdominal obesity—which refers to the accumulation of fat around the abdominal area—has a stronger association with the development of a hiatal hernia than general obesity. This is because the excess abdominal fat exerts more pressure on the stomach and diaphragm, which increases the risk of the stomach bulging upward into the chest.
Visceral fat, the type of fat that surrounds internal organs in the abdominal cavity, has been shown to be particularly problematic in contributing to hiatal hernias. Studies have found that visceral fat is more strongly associated with both GERD and hiatal hernias than subcutaneous fat (fat located just beneath the skin).
Increased Pressure from Abdominal Fat
The excess fat in the abdominal region is not only a source of physical pressure on the stomach but also contributes to increased pressure during activities like coughing, lifting heavy objects, or even when a person simply bends over. This heightened pressure can increase the likelihood of a hiatal hernia forming, particularly in individuals who are already at risk due to other factors such as age, smoking, or genetic predisposition.
3. How Obesity Aggravates the Symptoms of Hiatal Hernia
In addition to contributing to the formation of a hiatal hernia, obesity can also exacerbate the symptoms associated with the condition. The combination of increased intra-abdominal pressure and weakened diaphragm muscles makes it more likely that individuals who are obese will experience the following complications:
Gastroesophageal Reflux Disease (GERD)
GERD is a common condition among individuals with both obesity and a hiatal hernia. Obesity increases the risk of GERD due to the increased abdominal pressure and the weakened LES, which results from both the excess weight and the strain on the diaphragm. GERD leads to chronic heartburn, regurgitation, and discomfort, and it can lead to more severe complications if left untreated.
Worsening Heartburn and Acid Reflux
Obesity can significantly worsen the symptoms of heartburn and acid reflux, which are commonly associated with hiatal hernias. The added pressure from abdominal fat can push stomach contents, including acid, upward into the esophagus, causing a burning sensation in the chest and throat. In severe cases, this acid can cause inflammation and damage to the esophagus, leading to esophagitis, ulcers, and even an increased risk of esophageal cancer.
Difficulty Swallowing (Dysphagia)
As the stomach herniates upward into the chest, it can also cause difficulty swallowing (dysphagia) in some individuals. This occurs because the herniated stomach can obstruct the passage of food through the esophagus, leading to a sensation of food getting stuck in the throat. Obesity increases the likelihood of experiencing dysphagia, as the excess fat may contribute to increased pressure on the stomach and esophagus, making it harder to swallow food comfortably.
4. Managing Obesity to Prevent or Alleviate a Hiatal Hernia
Since obesity is a key risk factor for the development of a hiatal hernia, managing body weight is one of the most effective ways to prevent or reduce the severity of the condition. In individuals who already have a hiatal hernia, losing weight can help alleviate symptoms and prevent complications.
Diet and Exercise
Adopting a balanced diet and engaging in regular physical activity are essential steps in managing obesity. Weight loss can reduce the abdominal pressure that contributes to the formation and worsening of a hiatal hernia. A combination of cardiovascular exercise (such as walking, running, or swimming) and strength training can help reduce visceral fat and improve overall health.
A diet rich in fruits, vegetables, whole grains, and lean proteins, while low in processed foods, sugars, and unhealthy fats, can promote healthy weight loss and prevent further complications associated with obesity and hiatal hernias.
Reducing Intra-Abdominal Pressure
To help reduce intra-abdominal pressure, individuals with a hiatal hernia should avoid heavy lifting, excessive bending, or straining during bowel movements. These activities can increase the risk of the stomach being pushed up into the chest. Practicing good posture and maintaining an upright position after meals can also help reduce pressure on the stomach.
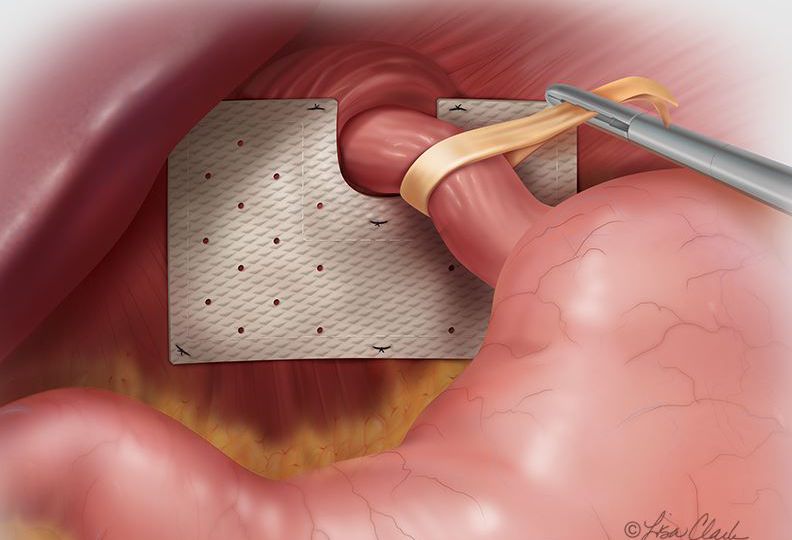
Surgical Intervention for Severe Cases
In cases where lifestyle changes are not enough to manage a hiatal hernia, and the symptoms are severe, surgical options may be considered. Procedures such as laparoscopic fundoplication or hiatal hernia repair may be used to correct the hernia, reduce the risk of complications, and provide relief from chronic GERD and other symptoms.
Obesity is a significant risk factor for the development of a stomach hernia (hiatal hernia). The relationship between obesity and hiatal hernias is largely due to increased abdominal pressure, the weakening of the diaphragm, and the relaxation of the lower esophageal sphincter, all of which contribute to the herniation of the stomach into the chest cavity. People with obesity, especially those with abdominal fat, are more likely to develop a hiatal hernia and experience worsening symptoms such as acid reflux, heartburn, and difficulty swallowing.
Managing obesity through diet, exercise, and lifestyle changes is one of the most effective ways to prevent the formation of a hiatal hernia or reduce the severity of symptoms in individuals already diagnosed with the condition. In more severe cases, surgical intervention may be necessary to correct the hernia and prevent further complications.
By understanding the relationship between obesity and hiatal hernias, individuals can take proactive steps to reduce their risk, improve their health, and enhance their quality of life.