1. Understanding GIST Recurrence and Metastasis
Before delving into the specifics of risk assessment, it is important to understand what recurrence and metastasis mean in the context of GISTs:
- Recurrence refers to the reappearance of a GIST after initial treatment, often following surgical resection. A tumor may recur locally in the same location or in nearby tissues, leading to a relapse of disease.
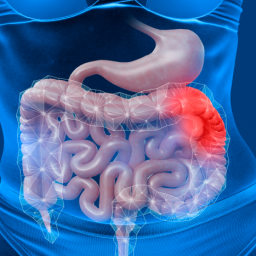
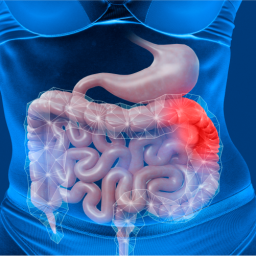
- Metastasis refers to the spread of cancer cells from the original tumor site to distant organs or lymph nodes. The most common sites for GIST metastasis include the liver and peritoneum (the lining of the abdominal cavity).
Both recurrence and metastasis can significantly impact a patient’s prognosis and treatment options. Identifying the risk factors early allows for personalized treatment planning, increasing the chances of successful management.
2. Risk Factors for GIST Recurrence and Metastasis
The risk of recurrence and metastasis in GIST patients depends on several factors, ranging from the size and location of the tumor to molecular characteristics. Key risk factors include:
a. Tumor Size

- Tumor size is one of the most important prognostic factors in predicting the risk of recurrence and metastasis in GIST patients. Larger tumors, especially those greater than 5 cm, are associated with a higher likelihood of metastasis and recurrence. Tumors that are smaller in size have a relatively lower risk of recurrence, though this does not eliminate the possibility altogether.
- Size and aggressiveness: Larger tumors may have more aggressive biological behavior and may be more likely to have spread to other organs or tissues by the time of diagnosis.
b. Tumor Location
- The location of the tumor within the GI tract plays a significant role in determining the risk of metastasis. Tumors in the stomach or small intestine are more common and tend to have a better prognosis than those located in the esophagus, colon, or rectum. GISTs located in the stomach are more likely to be benign, while those in the small intestine or other areas are more likely to be malignant and metastasize.
c. Mitotic Rate
- The mitotic rate refers to how quickly the tumor cells are dividing. A higher mitotic rate is associated with a more aggressive tumor that is more likely to metastasize or recur. The mitotic count is typically measured as the number of dividing cells seen in a high-power field under a microscope.
- Mitotic index: A mitotic rate of more than 5 mitoses per 50 high-power fields (HPF) is considered high and is a red flag for higher risk of recurrence and metastasis. This factor is particularly critical in determining whether adjuvant therapy with medications such as imatinib should be considered.
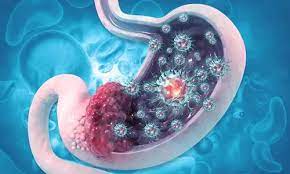
d. Tumor Cell Necrosis
- The presence of necrosis (dead tissue) within the tumor may also indicate a higher risk of metastasis. Necrotic tumors tend to have poor blood supply and are often more aggressive. The degree of necrosis is often evaluated during histopathological examination.
e. C-kit Mutation and Other Molecular Markers
- C-kit mutations (particularly in exon 11) are one of the most significant molecular markers in GISTs. GISTs that have mutations in the c-kit gene are more likely to respond to targeted therapies such as imatinib, but the mutation status can also give insight into the tumor’s aggressiveness.
- Other mutations: GISTs can also harbor mutations in the PDGFRA (platelet-derived growth factor receptor alpha) gene, and tumors with these mutations may behave differently from those with c-kit mutations. Understanding these genetic alterations can help predict the likelihood of recurrence and metastasis.
- Immunohistochemistry: Immunohistochemistry testing can be used to identify c-kit or PDGFRA expression on the surface of tumor cells, providing insight into the tumor’s molecular behavior and guiding therapeutic decisions.
f. Surgical Margins
- The surgical margin refers to the amount of healthy tissue surrounding the tumor that is removed during surgery. Incomplete resection or positive margins (tumor cells remaining at the surgical edge) significantly increase the risk of recurrence. A negative surgical margin (no tumor cells at the edge of the removed tissue) is associated with a lower risk of recurrence.
- Complete Resection: Achieving a complete resection with negative margins is crucial in reducing the risk of recurrence, although it does not guarantee that metastasis will not occur.
3. Assessment Methods for GIST Recurrence and Metastasis
Several assessment tools and techniques are used to evaluate the risk of recurrence and metastasis in GIST patients. These methods combine clinical, pathological, and molecular evaluations.
a. Histopathological Examination
- Histopathology, the microscopic examination of tissue, remains one of the most important ways to assess the risk of recurrence and metastasis. After a tumor is surgically removed, pathologists examine the tissue to evaluate factors such as tumor size, mitotic rate, necrosis, and molecular markers.
- Risk Stratification: Pathologists can categorize GISTs into different risk groups (low, intermediate, and high) based on these characteristics, helping doctors assess the likelihood of recurrence or metastasis. Tumors classified as high-risk typically require more aggressive treatment and closer follow-up.
b. Imaging Studies
- Imaging plays a critical role in monitoring the tumor’s behavior over time and identifying any recurrence or spread. Common imaging techniques used for GIST follow-up include:
- CT scans: To evaluate the size, location, and spread of the tumor, particularly to detect metastasis in the liver or peritoneum.
- MRI: Sometimes used for further evaluation of abdominal and pelvic tumors, especially when CT scan results are inconclusive.
- PET scans: PET scans combined with CT (PET-CT) can help identify areas of increased metabolic activity that may indicate metastasis.
c. Molecular Testing
- Molecular testing is becoming increasingly important in assessing GIST recurrence and metastasis. Genetic testing for mutations in the c-kit or PDGFRA genes can reveal information about the tumor’s aggressiveness and guide treatment decisions.
- Gene Sequencing: Advanced molecular testing, such as next-generation sequencing (NGS), can identify specific mutations and provide insight into the risk of recurrence or metastasis.
d. Follow-up Protocols
- Regular follow-up is essential for GIST patients after initial treatment. The frequency of follow-up visits and imaging tests depends on the risk level of recurrence. High-risk patients may undergo imaging every 3–6 months, while low-risk patients may be monitored less frequently.
- Follow-up duration: Follow-up may continue for several years after surgery, especially for high-risk patients, to detect recurrence early.
4. Clinical Implications and Treatment Strategies
Once the risk of recurrence and metastasis is assessed, it influences treatment decisions. For example, high-risk GIST patients may be offered adjuvant therapy with tyrosine kinase inhibitors (such as imatinib), which can help reduce the risk of recurrence by targeting c-kit or PDGFRA mutations. Similarly, patients with metastatic GIST may receive targeted therapy or undergo surgery for metastases.
5. Prognosis and Long-Term Management
The prognosis for GIST patients depends on a variety of factors, including the risk of recurrence and metastasis. Early detection, complete resection, and appropriate adjuvant therapies can significantly improve outcomes. Regular follow-up visits, including imaging and molecular tests, are essential for detecting recurrence or metastasis at the earliest stages.