
1. Effective Pain Management
One of the significant challenges for patients with esophageal cancer is managing pain and discomfort, especially when the tumor affects the ability to swallow or when treatment side effects, such as mouth sores or esophageal irritation, occur.
a. Medications

- Analgesics: Over-the-counter painkillers (such as ibuprofen or acetaminophen) and prescription medications like opioids (e.g., morphine or oxycodone) can provide significant relief. However, opioids should be used with caution, especially in the long term, as they can lead to dependence or other complications.
- Topical Analgesics: For those suffering from mouth sores or localized pain in the throat or esophagus, topical pain medications or mouth rinses containing lidocaine can offer temporary relief.
- Palliative Care: Palliative care teams are specialized in managing cancer-related symptoms, including pain. These professionals can provide expert care and adjust pain management plans based on the patient’s needs.
b. Non-Pharmacologic Pain Relief
- Acupuncture: Some patients find relief through acupuncture, which can help manage chronic pain and other symptoms.
- Physical Therapy: For patients recovering from surgery or radiation, physical therapy may help improve mobility and reduce discomfort caused by the cancer or its treatments.
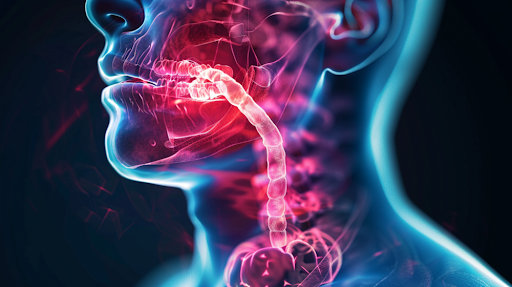
2. Managing Difficulty Swallowing (Dysphagia)
Difficulty swallowing is one of the hallmark symptoms of esophageal cancer and can drastically affect a patient’s ability to eat and maintain adequate nutrition. As the tumor grows, the esophagus narrows, making it harder for food and liquids to pass through.
a. Esophageal Dilation and Stenting
- Esophageal dilation is a procedure in which a balloon is used to stretch the esophagus, helping to alleviate the narrowing and make swallowing easier.
- Stents are sometimes placed in the esophagus to keep it open. These metal or plastic tubes can be inserted to prevent the esophagus from becoming too constricted, allowing patients to swallow more easily.
b. Swallowing Therapy
- Speech and Swallowing Therapists: Patients may benefit from working with a speech therapist who specializes in swallowing disorders. These professionals can teach patients techniques to improve swallowing safety and reduce the risk of choking or aspiration.
- Modified Diets: Patients may need to adopt soft or pureed food diets to make swallowing less challenging. Nutritional advice from a dietitian or nutritionist can ensure that patients receive the necessary nutrients while adapting to dietary changes.
3. Nutritional Support
Maintaining proper nutrition is one of the most important aspects of improving the quality of life for patients with esophageal cancer. Malnutrition and weight loss are common due to difficulty swallowing and reduced food intake, leading to weakness and fatigue.
a. Dietary Adjustments
- High-Calorie, High-Protein Foods: To combat weight loss and malnutrition, patients should focus on consuming calorie-dense and protein-rich foods. This includes options like whole milk, eggs, cream, lean meats, and protein shakes.
- Liquid Diets: If swallowing becomes extremely difficult, patients may rely on liquid meals or smoothies, fortified with nutrients, to ensure they are getting sufficient nutrition.
b. Enteral Nutrition (Feeding Tubes)
- For some patients who are unable to meet their nutritional needs through oral intake, enteral nutrition (via a feeding tube) may be recommended. This may involve a nasogastric (NG) tube or a gastrostomy tube (G-tube) to provide direct nourishment to the stomach. These tubes can help patients maintain weight and energy while they undergo treatment.
c. Nutritional Supplements
- For patients who struggle to consume enough calories and nutrients, liquid nutritional supplements (e.g., Ensure, Boost) can be a helpful option. These supplements provide essential vitamins, minerals, and macronutrients.
4. Psychosocial Support
The emotional and mental well-being of patients with esophageal cancer is just as important as their physical health. A cancer diagnosis can lead to anxiety, depression, and a sense of isolation, particularly as treatment can be long, difficult, and sometimes, disheartening.
a. Psychological Counseling
- Psychologists and counselors who specialize in cancer care can provide emotional support to patients. Cognitive-behavioral therapy (CBT) is one approach that can help manage the stress, anxiety, and depression associated with cancer.
- Support Groups: Joining a cancer support group allows patients to connect with others facing similar challenges. Sharing experiences and learning coping strategies can significantly reduce feelings of isolation and improve emotional well-being.
b. Mind-Body Therapies
- Yoga and Meditation: Many patients find that mindfulness practices, such as meditation and yoga, help reduce stress and improve their emotional health. These techniques can promote relaxation, improve sleep quality, and reduce anxiety.
- Breathing Exercises: Deep breathing exercises can help with anxiety and improve overall mood. These techniques are often recommended by cancer care teams as part of a holistic approach to well-being.
5. Improving Physical Function and Mobility
Physical activity can play a critical role in enhancing the quality of life for patients with esophageal cancer. Cancer treatment often results in fatigue and muscle weakness, which can make it harder for patients to perform everyday tasks.
a. Physical Therapy and Rehabilitation
- Patients recovering from surgery or radiation therapy may benefit from physical therapy to regain strength, improve mobility, and restore physical function.
- Exercise Programs: Tailored, low-impact exercise programs can help patients maintain their physical strength and reduce fatigue. Regular exercise can boost energy levels, improve mood, and promote overall health.
b. Fatigue Management
- Energy Conservation Techniques: Cancer patients often experience fatigue, which can interfere with daily activities. Occupational therapists can teach patients energy conservation techniques, such as pacing activities and taking regular rest periods, to prevent exhaustion.
- Adequate Rest: Ensuring that patients get enough rest is critical to managing fatigue. This can involve both daytime naps and good sleep hygiene practices at night to improve the quality of rest.
6. Palliative and End-of-Life Care
For patients with advanced esophageal cancer, the goal of care may shift toward providing comfort and improving the quality of life during the later stages of illness.
a. Palliative Care
- Palliative care focuses on managing symptoms, relieving pain, and enhancing the patient’s comfort and quality of life, rather than attempting to cure the disease. A palliative care team may include doctors, nurses, social workers, and chaplains who address physical, emotional, and spiritual needs.
b. Hospice Care
- Hospice care is another form of end-of-life care that focuses on providing comfort and support for patients with terminal cancer. Hospice teams offer pain management, emotional support, and counseling for both patients and their families, ensuring that the final stages of life are as peaceful and dignified as possible.
7. Support for Caregivers
The quality of life for patients with esophageal cancer also depends on the support they receive from their caregivers. Family members or friends who care for patients may face emotional, physical, and financial challenges as they help manage the patient’s illness.
a. Caregiver Support Groups
- Like cancer patients, caregivers also benefit from joining support groups where they can share experiences, seek advice, and find emotional comfort.
- Respite Care: Respite care services allow caregivers to take breaks from their caregiving duties, ensuring they have time to rest and recharge.
b. Practical Assistance
- Caregivers may require help with daily tasks, such as meal preparation, transportation to appointments, and managing medications. Home health aides and community services can provide this support, reducing the burden on family caregivers.
Improving the quality of life for patients with esophageal cancer requires a multifaceted approach that addresses not just the physical aspects of the disease, but also the emotional, nutritional, and social needs of the patient. By focusing on pain management, nutritional support, physical function, psychological well-being, and palliative care, patients can experience a better quality of life, even as they navigate the challenges of treatment and recovery.
Support from healthcare professionals, caregivers, and family members is essential to helping patients maintain a sense of normalcy, dignity, and hope during their cancer journey. By utilizing a combination of therapies and treatments, both medical and supportive, patients with esophageal cancer can optimize their quality of life and improve their overall experience during this difficult time.

