1. Chronic Pain and Its Psychological Effects
Chronic pain is defined as pain that persists for more than three months, well beyond the expected time for healing. It can be debilitating, both physically and psychologically. The psychological impact of chronic pain is often overlooked, but it plays a crucial role in a patient’s experience of the condition and its management.
The Link Between Physical and Psychological Health
The relationship between chronic physical pain and psychological distress is well-established. Chronic pain often leads to a range of emotional responses, including:
- Depression: Ongoing pain can trigger or exacerbate feelings of sadness, hopelessness, and a general sense of being overwhelmed. The inability to perform regular activities and the constant discomfort can lead to a downward spiral of negative emotions.
- Anxiety: Fear of future pain, unpredictable flare-ups, and the inability to manage pain effectively can contribute to heightened anxiety. Patients may worry about their condition worsening or never fully resolving.
- Stress: Chronic pain places a significant stress burden on the body and mind. The body’s stress response system is activated, leading to increased levels of cortisol, which in turn exacerbates the pain cycle.
- Isolation: Individuals suffering from chronic pain may withdraw from social activities due to embarrassment, discomfort, or a lack of energy. This social isolation can lead to feelings of loneliness and alienation.
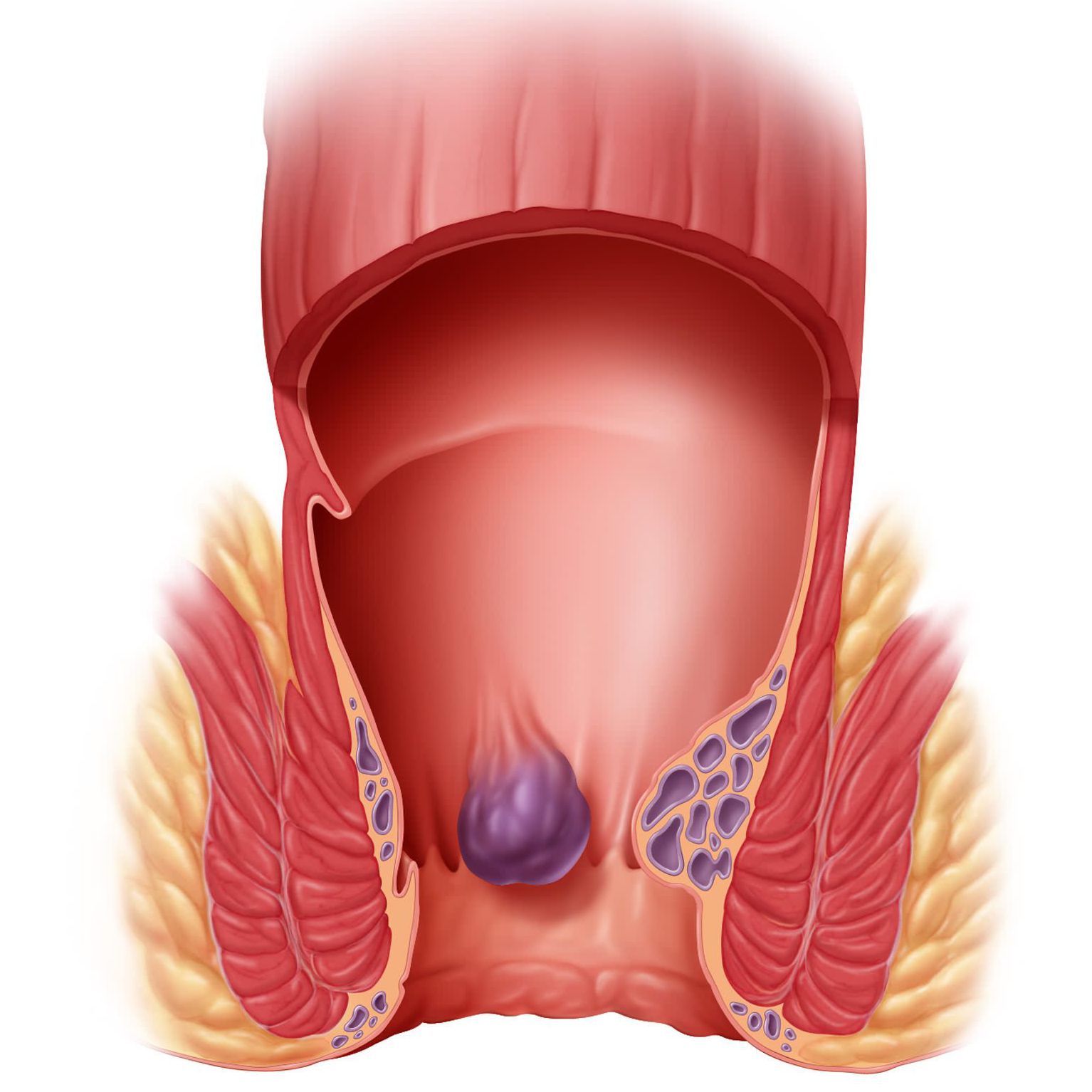
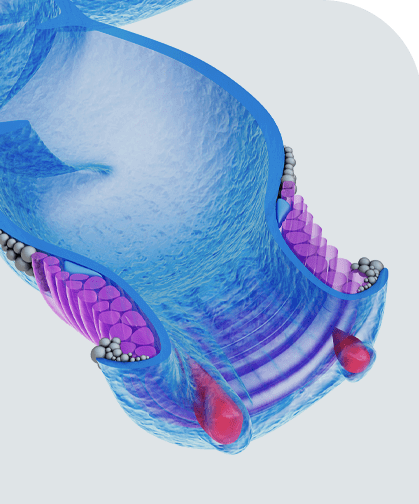
2. How Anal Fissures Contribute to Chronic Pain
An anal fissure, though often small, can cause intense pain. The pain is most commonly felt during or after a bowel movement, which can lead to anxiety surrounding the act of defecation. Over time, this pain can become chronic, particularly if the fissure does not heal properly or if it recurs. Anal fissures are commonly associated with:
- Severe pain: The pain associated with anal fissures is sharp, burning, or stabbing in nature and can last for hours, particularly after bowel movements. This persistent pain can be difficult to manage without proper treatment.
- Bleeding: While not as severe as the pain, the occasional bleeding caused by an anal fissure can contribute to anxiety and a heightened sense of distress, particularly if the individual has no prior experience with such symptoms.
- Emotional Toll of Constant Discomfort: The ongoing discomfort of anal fissures can affect an individual’s ability to focus, relax, or sleep, leading to further psychological distress.
3. Impact of Chronic Pain on the Quality of Life of Anal Fissure Patients
The psychological burden of chronic pain due to anal fissures significantly affects the overall quality of life. The quality of life (QoL) encompasses various aspects of a person’s life, including their emotional well-being, social life, physical health, and ability to function in daily tasks. Here’s how chronic anal fissure pain affects different aspects of a person’s life:
Emotional Well-Being
Chronic pain often leads to a reduced sense of well-being. The constant discomfort from an anal fissure can leave patients feeling frustrated, helpless, or defeated. Emotional reactions such as:
- Depression: The persistent pain can trigger depressive symptoms, with patients feeling sad or hopeless about their future. Depression in anal fissure patients may also manifest as a lack of motivation to engage in activities they once enjoyed.
- Anxiety: The fear of experiencing pain with every bowel movement or worrying about the condition worsening can lead to significant anxiety. This anxiety may affect patients’ ability to concentrate, leading to difficulties in work or daily activities.
- Anger and Irritability: Constant pain can make individuals irritable, angry, and short-tempered, especially when they feel misunderstood by others who may not fully grasp the severity of the condition.
Social and Interpersonal Impact
The impact of chronic anal fissure pain is not only felt physically and emotionally but can also affect a person’s social and interpersonal relationships. The following social impacts are common:
- Isolation: Because of the discomfort associated with anal fissures, individuals may avoid social situations, particularly those that involve long periods of sitting or eating. The embarrassment of having to explain the condition to others can make them withdraw socially.
- Strained Relationships: Chronic pain can cause frustration and tension in relationships, especially if one partner does not fully understand the challenges associated with the condition. This may lead to communication issues or emotional distance between partners.
- Reduced Work Performance: The pain may prevent individuals from focusing on work tasks, attending work regularly, or performing tasks efficiently. This can lead to job dissatisfaction, reduced career prospects, and financial stress.
Physical Limitations and Daily Functioning
Chronic pain from anal fissures can also impact a person’s physical functioning, affecting their ability to carry out everyday tasks. Anal fissure patients often experience:
- Difficulty Sitting: Pain while sitting is a common symptom of anal fissures, which can significantly affect a person’s ability to perform work tasks, attend meetings, or even engage in social activities that require prolonged sitting.
- Disrupted Sleep: The intense pain experienced during bowel movements or after them can affect sleep quality. Sleep disturbances, in turn, can lead to fatigue, reduced energy levels, and decreased concentration throughout the day.
- Hindrance to Physical Activity: The pain can also make physical activities like exercising or participating in hobbies difficult. The fear of exacerbating the fissure during activities can deter individuals from engaging in healthy practices, leading to physical deconditioning and weight gain.
4. Coping Mechanisms and Psychological Support for Anal Fissure Patients
Managing the psychological aspects of chronic pain is crucial in improving the quality of life of anal fissure patients. While addressing the physical symptoms of anal fissures is important, patients must also receive psychological support to cope with the emotional and mental toll.
Cognitive Behavioral Therapy (CBT)
CBT is a proven therapeutic approach for individuals dealing with chronic pain. By helping patients recognize and modify negative thought patterns related to pain, CBT can reduce anxiety, depression, and stress associated with the condition. CBT can teach patients how to manage pain by changing their perceptions and reactions to it, ultimately improving emotional well-being.
Mindfulness and Relaxation Techniques
Mindfulness techniques, such as meditation, deep breathing exercises, and progressive muscle relaxation, can be beneficial in reducing the mental strain of chronic pain. These practices help individuals remain focused in the present moment, reducing the tendency to ruminate on the pain. Mindfulness techniques can improve overall mood, decrease stress, and help manage anxiety.
Support Groups and Social Connection
Joining support groups for individuals with chronic pain or anal fissures can provide a sense of community and understanding. Sharing experiences with others who are going through similar challenges can reduce feelings of isolation and provide valuable coping strategies. Social support from friends, family, and healthcare providers is also essential in maintaining a positive outlook.
Pharmacological Treatment for Psychological Symptoms
In some cases, medications such as antidepressants or anti-anxiety drugs may be prescribed to manage the psychological symptoms associated with chronic pain. These medications can provide relief from symptoms of depression and anxiety, helping patients better manage their emotional well-being.
5. Improving the Quality of Life for Anal Fissure Patients
Improving the quality of life for individuals suffering from anal fissures involves both addressing the physical pain and providing psychological support. The following steps can help improve QoL for anal fissure patients:
- Early and Effective Treatment: Ensuring timely and effective treatment for anal fissures can prevent them from becoming chronic and reduce the duration of pain. Medical treatments may include topical creams, botox injections, or surgical intervention for severe cases.
- Patient Education: Educating patients about their condition, treatment options, and self-care practices can empower them to take control of their health, reducing feelings of helplessness.
- Physical Therapy: For some patients, pelvic floor physical therapy can help alleviate pain and muscle spasms related to anal fissures. A trained therapist can guide patients through exercises that relax the anal sphincter and reduce pain.
- Stress Management Techniques: Encouraging stress management strategies such as yoga, deep breathing exercises, and relaxation techniques can help mitigate the psychological impact of chronic pain.
The psychological impacts of chronic pain, particularly in the context of anal fissures, can have profound effects on a patient’s overall quality of life. The emotional toll, social isolation, and physical limitations imposed by chronic pain can lead to depression, anxiety, and stress, further exacerbating the condition. Addressing both the physical and psychological aspects of chronic anal fissure pain is essential for improving patient outcomes. Through effective treatment, psychological support, and lifestyle changes, individuals with anal fissures can regain control over their health, reduce their emotional distress, and improve their quality of life.