1. Overview of Focal Nodular Hyperplasia (FNH)
Focal Nodular Hyperplasia (FNH) is one of the most common benign lesions of the liver. It typically consists of a well-defined, localized area of liver tissue that has grown abnormally. The condition is characterized by the presence of a central scar, which is surrounded by normal liver tissue that has undergone hyperplastic (excessive growth) changes. FNH is not considered a cancerous condition, and it rarely causes any symptoms or health complications.
FNH is typically found in individuals between the ages of 20 and 50, with a higher prevalence in women, especially those who are on oral contraceptives or are pregnant. The cause of FNH is not completely understood, but it is believed to be related to a vascular abnormality, specifically an artery that supplies blood to the lesion.
2. Causes and Risk Factors of FNH
The exact cause of Focal Nodular Hyperplasia remains unclear. However, it is believed that it may be associated with a vascular anomaly within the liver. More specifically, FNH is thought to result from an abnormal blood vessel that supplies the lesion with blood, leading to hyperplasia (excessive growth) of the liver tissue.
Some potential risk factors and contributing elements for the development of FNH include:

- Hormonal Influence: FNH is more common in women than in men. The condition is often diagnosed in women of reproductive age, particularly those who take oral contraceptives or are pregnant, indicating that hormonal factors might play a role in the growth of these lesions.
- Vascular Abnormalities: FNH lesions are thought to arise due to an abnormal artery within the liver, which increases blood supply to the area, leading to the formation of hyperplastic tissue. This vascular malformation is typically responsible for the characteristic central scar seen in FNH.
- Genetic Factors: While FNH is generally considered non-hereditary, some cases have been observed in individuals with a family history of the condition. However, there is no clear genetic predisposition identified for FNH.
3. Symptoms of Focal Nodular Hyperplasia
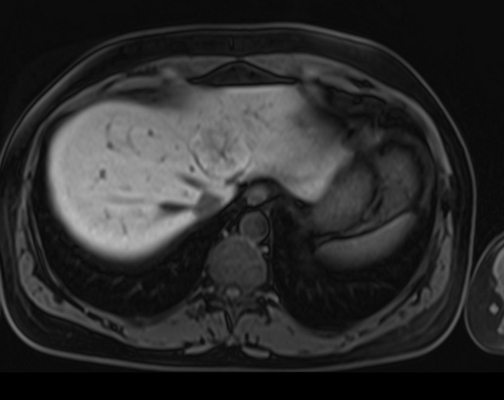
Focal Nodular Hyperplasia is often asymptomatic, meaning that many people who have FNH may not experience any noticeable symptoms. In most cases, it is discovered accidentally during imaging studies like ultrasounds, CT scans, or MRIs, performed for other medical reasons.
In some rare cases, individuals with FNH may experience symptoms, which include:
- Abdominal Pain or Discomfort: This may occur if the lesion is large or if it causes pressure on surrounding tissues or organs.
- Hepatomegaly: Enlargement of the liver, which might be detectable during a physical examination, can occur in some cases of FNH.
- Jaundice: Although rare, a large lesion could affect the bile ducts, leading to bile flow obstruction and jaundice (yellowing of the skin and eyes).
- Nausea and Vomiting: These symptoms are also rare but may occur if the lesion affects liver function or other nearby organs.
Despite these potential symptoms, most individuals with FNH do not experience any discomfort or adverse effects, and the condition typically requires no medical intervention.
4. How is FNH Diagnosed?
FNH is often diagnosed incidentally during routine imaging studies, as most people do not experience symptoms. The diagnostic process typically begins with the patient undergoing imaging tests for other unrelated health concerns. If a liver lesion is detected, further evaluation is necessary to differentiate between benign lesions like FNH and malignant conditions such as liver cancer or metastasis.
A. Imaging Tests

- Ultrasound: A liver ultrasound is usually the first imaging test used to detect liver abnormalities. FNH lesions typically appear as well-defined, hypoechoic (darker on the ultrasound) masses that are often distinct from surrounding tissue.
- CT Scan (Computed Tomography): CT scans are more detailed than ultrasounds and can provide a clearer image of the liver and any lesions. In cases of FNH, a CT scan may show a central scar surrounded by normal liver tissue.
- MRI (Magnetic Resonance Imaging): MRI is particularly useful in diagnosing FNH because it offers superior detail of soft tissue structures. It can help identify the central scar that is characteristic of FNH. Contrast agents may be used to enhance the clarity of the lesion.
- Angiography: In some cases, an angiogram may be performed to visualize the blood vessels within the lesion. FNH typically shows a vascular pattern with a central artery feeding into the lesion, which is an essential diagnostic feature.
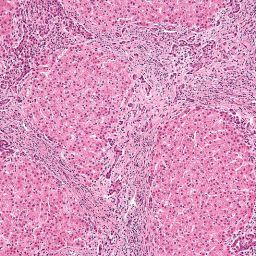
B. Biopsy
Although imaging studies can provide a clear picture of FNH, a biopsy (taking a sample of liver tissue for examination) is rarely necessary because FNH is benign and the diagnosis can usually be made based on imaging. A biopsy may be performed if there is uncertainty in the diagnosis or if there is suspicion of malignancy.
5. Treatment Options for Focal Nodular Hyperplasia
Focal Nodular Hyperplasia is generally a benign condition that does not require treatment. In most cases, no intervention is needed, and the patient can simply be monitored over time. However, treatment may be recommended in specific circumstances.
A. Observation and Monitoring
For most people with FNH, the best course of action is to observe the lesion and monitor it periodically. Regular imaging tests are often used to ensure that the lesion is not growing or causing any complications. As FNH is typically asymptomatic, people can usually lead normal lives without the need for medical intervention.
Monitoring may be particularly important for individuals who experience mild symptoms, or for those with larger lesions or complex lesions that may require further assessment.
B. Surgical Intervention
Surgery is rarely needed for FNH, but it may be considered in certain situations, such as:
- Symptoms: If a large FNH lesion causes significant pain or discomfort, or if it impairs liver function, surgical removal may be an option.
- Diagnostic Uncertainty: If there is uncertainty in the diagnosis and the lesion cannot be definitively identified as FNH, surgery may be performed to remove the lesion for further examination.
- Cosmetic or Aesthetic Concerns: In some cases, particularly when FNH lesions are large or visibly affecting liver appearance, patients may choose to have the lesion surgically removed for cosmetic reasons.
The surgical procedure typically involves the removal of the lesion, and in some cases, a portion of the surrounding liver tissue may also be removed. However, surgery is usually reserved for cases where the benefits outweigh the risks, as FNH is generally not harmful.
C. Medications
Currently, there are no specific medications for treating FNH. If a patient is experiencing symptoms related to FNH, such as abdominal pain or discomfort, medications such as pain relievers or anti-inflammatory drugs may be prescribed to manage symptoms. Hormonal therapies or oral contraceptives may be adjusted if they are thought to be contributing to the development or growth of FNH.
6. Complications and Prognosis
The prognosis for individuals with FNH is generally excellent, as the condition is benign and rarely causes serious health problems. Most patients can continue with their daily activities without any limitations. FNH does not lead to liver cancer or other complications in the vast majority of cases.
However, in rare instances, complications may arise:
- Large Lesions: Although uncommon, large FNH lesions may lead to discomfort or functional impairments in the liver or surrounding organs.
- Misdiagnosis: Since FNH can appear similar to other liver conditions such as tumors, there is a small risk of misdiagnosis, which may lead to unnecessary treatment or interventions.
- Bleeding: If the FNH lesion is particularly large or vascular, there is a small risk of bleeding. However, this is a rare occurrence.
Focal Nodular Hyperplasia (FNH) is a benign liver lesion that typically poses no significant health risks. It is most often asymptomatic and discovered incidentally during imaging tests. FNH can be managed effectively with observation and periodic monitoring, and surgical intervention is rarely necessary unless complications arise or the lesion grows to an unusual size.
As with any health condition, it is important for individuals with FNH to consult their healthcare provider for a personalized plan of action. Regular imaging tests can help ensure that the condition does not cause further problems, and timely interventions can be made when necessary. With proper management, people with FNH can generally lead a normal, healthy life.