What Causes the Formation of Liver Cysts?
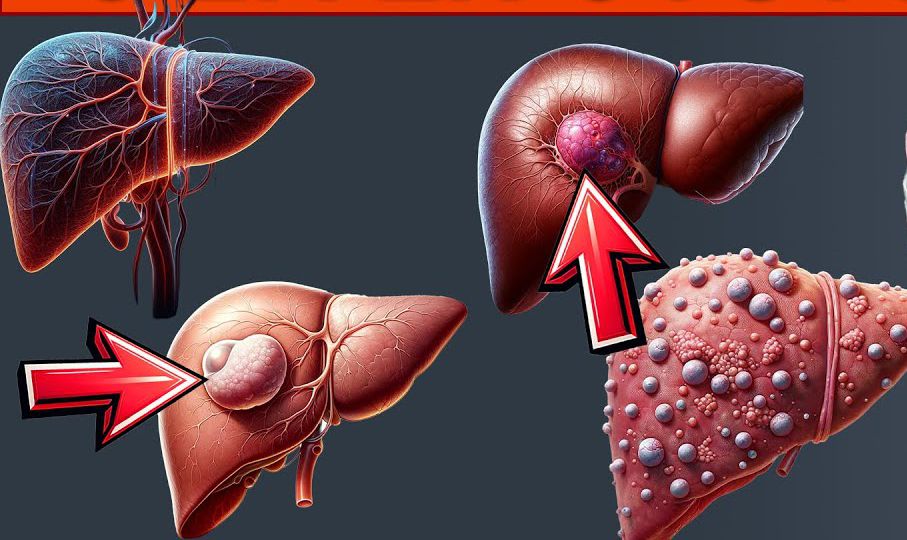
Liver cysts are fluid-filled sacs that develop within the liver, and although they are typically benign, their presence can sometimes lead to discomfort and medical concerns. Understanding the underlying causes of liver cysts is crucial for diagnosing the condition, determining treatment options, and managing potential complications. This article will explore the various causes of liver cysts, including congenital factors, infections, lifestyle influences, and more, providing a comprehensive overview of how these cysts develop and the medical implications they carry.
1. Congenital Factors: Primary Liver Cysts

Congenital liver cysts are those that develop during fetal development and are typically present at birth. The cause of these cysts is often unknown, though it is believed that they occur due to abnormal development of bile ducts during early stages of liver formation. These cysts are usually referred to as simple liver cysts and are often asymptomatic, meaning that individuals may have them for years without realizing it.
Congenital liver cysts can vary in size and may be singular or multiple. The majority of these cysts do not cause significant medical problems and are usually found incidentally during imaging tests for unrelated conditions. However, in some cases, they may grow large enough to cause symptoms like pain or pressure on adjacent organs.
2. Polycystic Liver Disease (PLD)
Polycystic liver disease (PLD) is a genetic disorder that causes multiple cysts to form in the liver. It is usually inherited in an autosomal dominant pattern, meaning that if a person has one affected parent, there is a 50% chance of inheriting the condition. PLD is often associated with polycystic kidney disease (PKD), a condition where multiple cysts also form in the kidneys.
In PLD, cysts grow progressively over time and can vary in size, sometimes affecting liver function if the cysts become too large. The cause of cyst formation in PLD is related to genetic mutations that interfere with the normal development of liver cells. These mutations lead to the formation of fluid-filled sacs within the liver. PLD can remain asymptomatic in the early stages, but as the disease progresses, it may cause symptoms such as abdominal pain, nausea, and a feeling of fullness due to the liver’s enlarged size.
3. Acquired Liver Cysts
Unlike congenital cysts, acquired liver cysts develop later in life. These types of cysts are often caused by various factors, such as infections, inflammation, and certain diseases. Acquired liver cysts can be further categorized based on the underlying causes.
A. Parasitic Infections (Echinococcosis)
One of the most notable causes of acquired liver cysts is parasitic infection, specifically echinococcosis or hydatid disease. This infection is caused by tapeworms, specifically Echinococcus species, which are transmitted to humans through contact with infected animals such as dogs. The larvae of the tapeworms can form cysts in the liver, lungs, and other organs, with the liver being the most common site.
Hydatid cysts are often large, and the infection can cause significant symptoms, including abdominal pain, fever, and jaundice. In some cases, the cysts may rupture, leading to severe complications such as anaphylaxis, infection, or bile leakage. Treatment for hydatid cysts typically involves medication, such as albendazole, and in many cases, surgical removal of the cysts.
B. Biliary Cystadenomas
Biliary cystadenomas are rare benign tumors that arise from the bile ducts and can lead to the formation of cysts within the liver. These cysts are typically larger than simple cysts and can grow progressively over time. They can cause symptoms such as abdominal discomfort, jaundice, and nausea, particularly if they block the bile ducts or interfere with liver function.
While biliary cystadenomas are typically benign, they can sometimes develop into malignant tumors, a condition known as biliary cystadenocarcinoma. As such, these cysts are closely monitored through imaging and may require surgical removal if they show signs of malignancy or cause significant symptoms.
C. Cystic Degeneration of Liver Tumors
In some cases, liver tumors, including hemangiomas, adenomas, and hepatocellular carcinoma (HCC), may undergo a process known as cystic degeneration. This occurs when parts of a tumor become cystic due to changes in blood flow, necrosis (tissue death), or other pathological factors. Cystic degeneration can result in fluid-filled spaces within the tumor, giving the appearance of a cyst on imaging scans.
The presence of cysts within liver tumors may make diagnosis more complicated, as these cysts can mimic benign conditions. Therefore, a thorough evaluation of the patient’s medical history, physical examination, and imaging studies is necessary to differentiate between benign liver cysts and tumors that may require further treatment, such as surgery or biopsy.
4. Infections and Inflammatory Conditions

Infections and inflammatory conditions that affect the liver can sometimes lead to the development of cysts. One example is liver abscesses, which are typically caused by bacterial, fungal, or parasitic infections. When an abscess forms in the liver, it can create a fluid-filled cavity similar to a cyst.
Liver abscesses can result from infections originating in other parts of the body, such as the gallbladder, intestines, or pancreas, and may cause symptoms such as fever, chills, abdominal pain, and nausea. Treatment typically involves antibiotics or antifungal medications, and in some cases, surgical drainage may be required.
Additionally, autoimmune hepatitis and other inflammatory liver diseases can contribute to the formation of cyst-like structures in the liver. Inflammation in the liver can cause tissue damage and lead to the formation of fluid-filled cavities.
5. Liver Injury and Trauma
In rare cases, liver cysts can develop after injury or trauma to the liver. If the liver is injured, it may lead to the formation of a hematoma (a collection of blood) within the liver tissue, which can later evolve into a cyst as the blood is reabsorbed. Traumatic liver cysts may not appear immediately after the injury but can be detected during follow-up imaging studies.
In such cases, the cyst is typically a result of the body’s healing process, and most cysts related to liver injury do not cause significant problems. However, they may need monitoring to ensure that they do not grow or lead to further complications, such as infection or rupture.
6. Hormonal Influence
Hormonal changes, particularly those related to estrogen, have been linked to the development of certain types of liver cysts. For example, liver adenomas (benign tumors of the liver) are more common in individuals with higher levels of estrogen, such as women who take oral contraceptives or who are pregnant. These adenomas may sometimes contain cyst-like structures within them, especially in the context of hormonal changes.
Although liver adenomas are generally benign, they can grow large and may pose risks if they rupture or cause bleeding. In such cases, treatment options may include surgical removal, especially if the adenoma is symptomatic or presents a risk of malignancy.
7. Lifestyle Factors and Liver Disease
Certain lifestyle factors, including alcohol abuse, poor diet, and obesity, may contribute to the development of liver disease and, in turn, increase the risk of liver cyst formation. Chronic alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), and cirrhosis can cause damage to the liver tissue, leading to scarring and the development of cysts or cyst-like lesions in the liver.
Liver damage from these conditions can increase the likelihood of cyst formation, particularly if the liver is severely damaged or scarred. In some cases, cirrhosis can lead to the development of biliary cysts or bile duct cysts, which can disrupt liver function.
Liver cysts are generally benign growths that can develop due to a variety of causes, from congenital factors to acquired conditions. In most cases, they do not cause symptoms and may not require treatment. However, in some instances, liver cysts can grow large or lead to complications that necessitate medical intervention. Identifying the underlying cause of liver cysts is essential for determining the best approach to treatment, as different causes may require different management strategies.
For individuals diagnosed with liver cysts, regular monitoring and follow-up imaging may be necessary to ensure that the cysts do not grow or cause problems. In cases where symptoms arise or complications develop, treatment options such as medication or surgery may be considered. By understanding the causes and implications of liver cysts, individuals can make informed decisions regarding their health and seek the appropriate care when necessary.


