Pathophysiology of Liver Adenomas
Liver adenomas develop when hepatocytes in the liver proliferate abnormally, leading to the formation of a mass. The growth of these tumors is often triggered by hormonal imbalances or genetic mutations. Typically, liver adenomas do not cause symptoms, and many are asymptomatic. They are most commonly diagnosed in young women, particularly those who use oral contraceptives or undergo hormone replacement therapy.
The benign nature of these tumors does not preclude the risks associated with their presence. Due to their vascularity, these adenomas are susceptible to bleeding, rupture, and, in rare cases, malignant transformation. To understand why liver adenomas may become cancerous, it is necessary to examine how these tumors evolve and the factors contributing to their malignancy.
Factors Contributing to Cancerous Transformation
Although the majority of liver adenomas remain benign, certain conditions make them more prone to becoming malignant. The risk of transformation is influenced by several key factors, such as tumor size, hormonal influence, genetic mutations, and the presence of pre-existing liver diseases.
1. Size and Growth Patterns
Liver adenomas that exceed a size of 5 cm carry a higher risk of complications, including malignant transformation. Larger adenomas, particularly those that are over 10 cm in diameter, present a significant risk for developing into hepatocellular carcinoma (HCC), the most common form of liver cancer. Studies indicate that as the size of an adenoma increases, the risk of malignancy escalates. Larger adenomas are more likely to have irregular growth patterns, blood vessel involvement, and characteristics that raise suspicion for cancerous changes.
2. Hormonal Influence
Hormonal factors play a critical role in the development and growth of liver adenomas. Women who use oral contraceptives or undergo hormone replacement therapy (HRT) have a significantly higher risk of developing liver adenomas. Estrogen, a key hormone in both contraceptives and HRT, can stimulate the growth of these benign tumors. It is also thought that long-term exposure to high levels of estrogen can lead to the malignant transformation of adenomas.
Hormonal changes during pregnancy can also influence the growth of liver adenomas. Studies have shown that pregnancy hormones, particularly progesterone, can lead to the enlargement of existing adenomas. Furthermore, women with a history of prolonged use of oral contraceptives are more likely to develop multiple adenomas, which increases the risk of complications, including malignant transformation.
3. Genetic Factors and Mutations
Genetics play a significant role in the development and malignancy of liver adenomas. Patients with certain inherited conditions such as familial adenomatous polyposis (FAP) and glycogen storage diseases are at a higher risk of developing multiple liver adenomas. These genetic disorders lead to abnormal cell growth, which can increase the likelihood of malignant transformation.
Additionally, mutations in certain genes, particularly the beta-catenin gene, have been linked to an increased risk of malignancy. Beta-catenin is involved in the Wnt signaling pathway, which regulates cell growth and differentiation. Mutations in this gene can disrupt normal cellular processes, leading to abnormal growth patterns and increasing the likelihood of cancer.
4. Underlying Liver Diseases
Individuals with chronic liver diseases such as cirrhosis, non-alcoholic fatty liver disease (NAFLD), hepatitis B or C, and other forms of chronic liver inflammation are at a higher risk of developing liver cancer. Chronic liver conditions cause continuous liver cell damage, which may promote the formation of tumors, including liver adenomas. If these adenomas form in the context of pre-existing liver diseases, the risk of malignancy is amplified.
In these individuals, the liver’s ability to repair itself is compromised, creating an environment conducive to the growth of abnormal cells. Furthermore, chronic liver inflammation can alter the liver’s cellular environment, making it more likely for benign tumors to become cancerous.
How Can Malignant Transformation Be Monitored?
Surveillance of liver adenomas is essential to detect any early signs of malignant transformation. Since most adenomas remain asymptomatic and benign, regular monitoring allows for early detection of potential complications. Several diagnostic tools and imaging techniques are used to monitor the size, growth, and characteristics of liver adenomas.
1. Imaging Techniques
Imaging plays a pivotal role in the diagnosis and monitoring of liver adenomas. The following imaging techniques are commonly used:
- Ultrasound: Often the first imaging method used to detect liver adenomas, ultrasound provides a quick and cost-effective way to visualize liver masses. However, it is less specific compared to other imaging methods and may require further investigation.
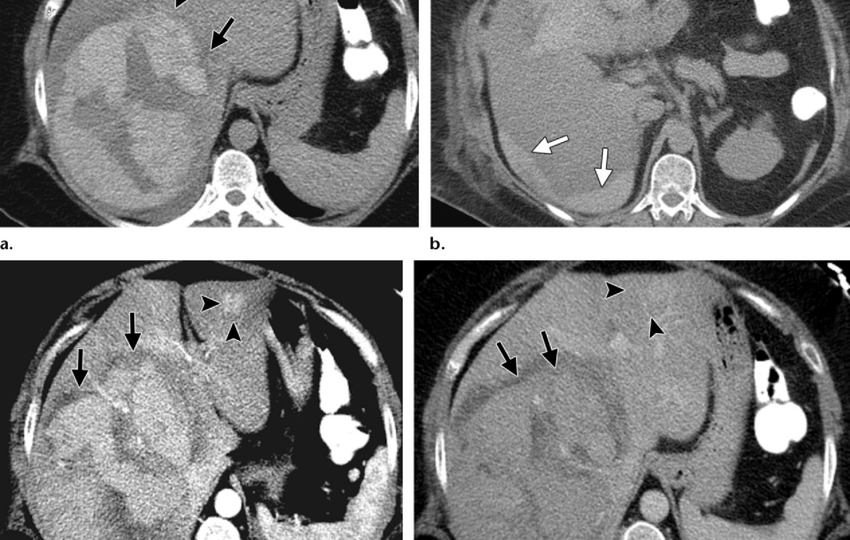
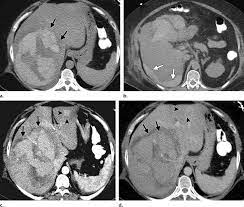
- CT Scans: Computed tomography (CT) scans offer a more detailed look at liver adenomas, including their size, location, and vascular characteristics. Contrast-enhanced CT scans allow for more accurate detection of abnormal growth patterns or other changes that might suggest the onset of malignancy.
- MRI: Magnetic resonance imaging (MRI) is considered the most effective imaging technique for liver adenomas. MRI provides high-resolution images that allow for an accurate assessment of the adenoma’s size, shape, and blood vessel involvement. This technique is particularly useful for identifying subtle changes in the tumor that might indicate malignant transformation.
2. Biopsy and Histopathological Examination
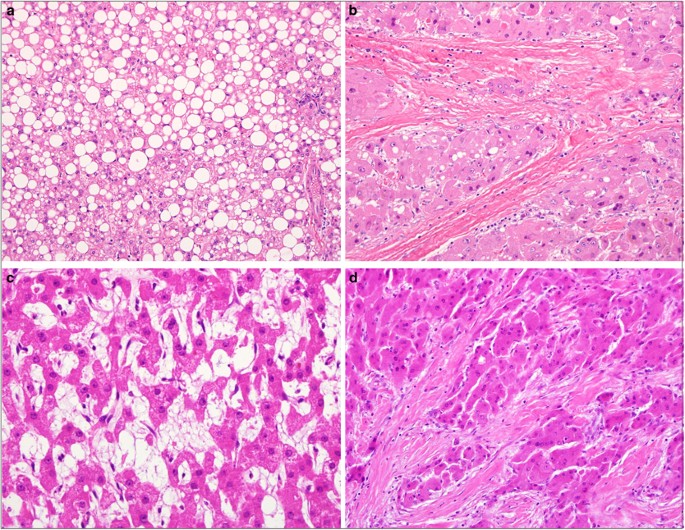
In some cases, when imaging studies suggest possible malignancy or if the adenoma shows irregular growth patterns, a liver biopsy may be recommended. During a biopsy, a small sample of tissue is removed from the adenoma for histopathological examination. This examination allows for the identification of cancerous cells and provides a definitive diagnosis of malignancy.
Biopsy is generally reserved for cases where there is uncertainty regarding the benign nature of the adenoma. Although a liver biopsy carries some risks, such as bleeding and infection, it remains a critical tool in diagnosing liver cancer.
What Are the Treatment Options for Malignant Liver Adenomas?
In rare cases, when liver adenomas undergo malignant transformation and develop into hepatocellular carcinoma (HCC), treatment options depend on several factors, including the tumor’s size, location, and the presence of any underlying liver conditions.

1. Surgical Resection
If a liver adenoma becomes cancerous but remains localized, surgical resection may be the preferred treatment. During this procedure, the tumor is removed along with a portion of the surrounding healthy liver tissue. Surgical resection is typically recommended if the tumor is confined to one area and has not spread to other parts of the liver or body. Early resection can significantly improve the prognosis and prevent the cancer from spreading further.
2. Liver Transplantation
In cases where the cancer has spread beyond the liver or if the liver is severely damaged due to pre-existing liver disease, liver transplantation may be necessary. During a liver transplant, the diseased liver is removed and replaced with a healthy donor liver. This option is generally reserved for patients with advanced liver cancer or those who have significant liver damage that impairs liver function.
3. Chemotherapy and Targeted Therapy
When surgery is not an option, or if the cancer has metastasized to other organs, chemotherapy and targeted therapy may be used. Chemotherapy aims to kill cancer cells or stop their growth, while targeted therapy involves using medications that target specific molecules involved in cancer cell growth.
These treatments are often used in conjunction with other interventions, such as liver transplantation, to provide a comprehensive approach to cancer treatment.
While liver adenomas are predominantly benign, they do carry the potential for malignant transformation, particularly in individuals with certain risk factors. The size of the adenoma, genetic predispositions, hormonal influences, and the presence of chronic liver diseases are critical factors in determining the likelihood of cancerous changes. Regular monitoring through imaging techniques, coupled with timely intervention, is essential for managing these tumors and reducing the risk of complications. If malignant transformation occurs, surgical resection, liver transplantation, and other cancer treatments may be necessary to improve patient outcomes and ensure the best possible prognosis.
By staying vigilant and closely monitoring liver adenomas, healthcare providers can help mitigate the risk of cancer and provide patients with the necessary care to manage their condition effectively.