1. The Importance of Early Detection of Liver Cancer
Liver cancer, particularly hepatocellular carcinoma (HCC), is one of the leading causes of cancer-related deaths globally. It is often diagnosed at an advanced stage due to the liver’s ability to compensate for damage until a substantial portion of the liver is affected. The lack of early symptoms makes it even more challenging to detect.
Early detection through screening allows for:
- Better treatment outcomes: When liver cancer is found early, patients may be eligible for surgery, liver transplant, or other curative treatments.
- Improved survival rates: Early-stage liver cancer has a better prognosis and can often be managed effectively.
- Minimizing the spread of cancer: Detecting liver cancer early can help prevent it from spreading to other organs.
However, not everyone needs to undergo liver cancer screening. Screening is most beneficial for those at higher risk, such as individuals with cirrhosis, chronic hepatitis, or a family history of liver cancer.
2. Who Should Consider Screening for Liver Cancer?
The primary goal of liver cancer screening is to identify the disease in individuals who are at an elevated risk. While screening may not be necessary for everyone, certain populations are more likely to benefit from regular testing. These include:
2.1 Individuals with Chronic Liver Disease
People who suffer from chronic liver diseases, especially those caused by hepatitis B or C, are at a significantly higher risk of developing liver cancer. Hepatitis B and C are major causes of liver cirrhosis, which in turn increases the risk of HCC. Regular screening is crucial for these individuals.

- Chronic Hepatitis B: People with chronic hepatitis B (HBV) have a higher risk of developing liver cancer, particularly if the infection is not well controlled. Screening is recommended every six months to detect liver cancer early.
- Chronic Hepatitis C: Hepatitis C (HCV) infection leads to liver inflammation, which can progress to cirrhosis and eventually liver cancer. Screening for liver cancer is recommended for individuals with long-standing HCV infections.
2.2 People with Cirrhosis
Cirrhosis is the scarring of liver tissue caused by liver damage from chronic diseases, alcohol use, or viral infections. This damage can eventually lead to liver cancer. People diagnosed with cirrhosis are at a higher risk of developing liver cancer, even if they don’t have hepatitis.
- Alcoholic cirrhosis: Individuals who have cirrhosis due to heavy alcohol use should also undergo regular screening for liver cancer.
- Non-alcoholic fatty liver disease (NAFLD): Cirrhosis caused by NAFLD, often associated with obesity and diabetes, is becoming an increasingly common risk factor for liver cancer.
2.3 Family History of Liver Cancer
Genetics also plays a role in liver cancer risk. People with a family history of liver cancer or inherited liver diseases, such as hemochromatosis (excessive iron accumulation) or Wilson’s disease (copper accumulation), are at an increased risk. These individuals may benefit from regular screening starting at an earlier age.
2.4 Individuals with Diabetes and Obesity
Both diabetes and obesity are linked to an increased risk of liver cancer. Obesity leads to non-alcoholic fatty liver disease (NAFLD), which can progress to cirrhosis and liver cancer over time. People with type 2 diabetes are also at higher risk of developing liver cancer, particularly if they are overweight or obese.
3. Screening Tests for Liver Cancer
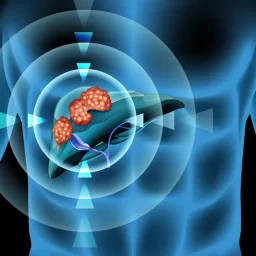
There are several screening tests used to detect liver cancer, most of which aim to identify tumors at an early, treatable stage. These tests primarily focus on detecting signs of liver cancer or liver damage that could indicate the potential for cancer development.
3.1 Ultrasound
Ultrasound is one of the most commonly used and non-invasive screening tools for liver cancer. It uses sound waves to create images of the liver, which can help detect tumors. A liver ultrasound is often recommended for individuals at high risk, particularly those with chronic hepatitis or cirrhosis.
- How it works: During the ultrasound, a gel is applied to the skin over the abdomen, and a small device called a transducer is moved over the area to create real-time images of the liver.
- Advantages: Ultrasound is relatively inexpensive, easy to perform, and does not involve radiation. It is also a good first-line screening tool for liver cancer.
- Limitations: While ultrasound can detect large tumors, it may not be sensitive enough to identify smaller cancers in the early stages.
3.2 Alpha-Fetoprotein (AFP) Blood Test
The alpha-fetoprotein (AFP) blood test measures the level of AFP, a protein that is often elevated in individuals with liver cancer, particularly in those with hepatocellular carcinoma (HCC). It is not a definitive test for liver cancer, but when used in conjunction with ultrasound, it can help increase the accuracy of early detection.
- How it works: A blood sample is drawn, and the AFP levels are measured in the lab. Elevated AFP levels can be a sign of liver cancer, but other conditions, such as cirrhosis or hepatitis, can also cause increased AFP.
- Advantages: The AFP test is simple, inexpensive, and can be used regularly for monitoring high-risk individuals.
- Limitations: Not all liver cancers produce elevated AFP levels, and elevated AFP can be seen in non-cancerous liver diseases as well.
3.3 CT Scan (Computed Tomography)
A CT scan is another imaging technique used to detect liver cancer, particularly if ultrasound and AFP testing suggest the presence of a tumor. CT scans provide more detailed images of the liver and can help determine the size, shape, and location of a tumor. This test is typically used if there is suspicion of liver cancer following other screening methods.
- How it works: The patient lies on a table that slides into a CT scanner. The scanner takes multiple X-ray images of the liver from different angles, and a computer combines them into cross-sectional images.
- Advantages: CT scans provide detailed images of the liver, allowing doctors to assess the size, shape, and extent of the tumor.
- Limitations: CT scans involve exposure to radiation, and they may not be recommended for routine screening unless needed for further diagnosis.
3.4 MRI (Magnetic Resonance Imaging)
MRI uses magnetic fields and radio waves to produce high-quality images of the liver. It is highly sensitive and can help detect liver tumors at an earlier stage compared to ultrasound. MRI can also provide more detailed information about the liver tissue, including signs of cirrhosis or fatty liver disease.
- How it works: The patient lies inside an MRI machine while it uses magnetic fields to create detailed images of the liver and surrounding organs.
- Advantages: MRI is non-invasive and provides highly detailed images without radiation. It is more effective than CT scans at identifying liver tumors.
- Limitations: MRI is more expensive than ultrasound and CT scans and is not typically used for routine screening in high-risk individuals unless required for further diagnosis.
3.5 Elastography (FibroScan)
Elastography (also known as FibroScan) is a technique that measures the stiffness of the liver tissue. It is useful for assessing liver damage and fibrosis, which is a precursor to cirrhosis and liver cancer. This non-invasive test is commonly used to monitor patients with chronic liver conditions, such as hepatitis and fatty liver disease, who are at higher risk of developing liver cancer.
- How it works: A small probe is placed on the abdomen, which sends sound waves into the liver. The speed at which the sound waves travel is measured, which correlates with the stiffness of the liver tissue.
- Advantages: Elastography is quick, non-invasive, and does not require a biopsy to assess liver stiffness.
- Limitations: It is not a definitive test for liver cancer but helps identify patients at risk due to liver damage or cirrhosis.
4. How Often Should Liver Cancer Screening Be Done?
The frequency of liver cancer screening depends on the individual’s risk factors, including the presence of cirrhosis, chronic hepatitis, or other liver conditions. Generally, individuals at high risk should undergo screening every 6 to 12 months.
- Chronic hepatitis B: Screening every 6 months with ultrasound and AFP is typically recommended.
- Chronic hepatitis C: Similar to hepatitis B, individuals with chronic hepatitis C should have regular screening, especially if they have cirrhosis.
- Cirrhosis: For those with cirrhosis, screening should also be done at least once every 6 months.
For those with a higher risk but no signs of cirrhosis or liver disease, a physician may recommend less frequent screening, depending on their overall health and medical history.
Liver cancer is a deadly disease, but early detection through regular screening can significantly improve outcomes and survival rates. Screening for liver cancer involves a combination of imaging tests such as ultrasound, CT, or MRI, along with blood tests like the AFP test. While these tests are not perfect, they can help identify liver cancer in high-risk individuals at an earlier stage when treatments are more effective.
Individuals with chronic liver diseases, cirrhosis, a family history of liver cancer, or certain lifestyle factors such as diabetes and obesity should consider undergoing regular liver cancer screenings. Consulting with a healthcare provider is essential to determine the most appropriate screening plan based on individual risk factors.
Regular screening, coupled with early intervention, can make a significant difference in managing liver cancer, leading to improved prognosis and quality of life for those affected.