1. Understanding Liver Cancer and Treatment Options
Liver cancer typically refers to two main categories: primary liver cancer (such as hepatocellular carcinoma, or HCC) and secondary liver cancer (cancer that has spread to the liver from other organs). Treatment for liver cancer can include surgery, liver transplantation, ablation techniques, chemotherapy, immunotherapy, targeted therapy, and radiation therapy.
However, liver cancer’s treatment often depends on a variety of factors, including the tumor’s size, location, stage, and whether the patient has underlying liver diseases like cirrhosis or chronic hepatitis. While surgery is often the first-line treatment, radiation therapy plays a crucial role in certain scenarios where surgery may not be feasible.
2. What is Radiation Therapy?
Radiation therapy uses high-energy radiation, typically in the form of X-rays, to target and destroy cancer cells. It works by damaging the DNA within the cancer cells, which prevents them from growing and dividing. Unlike chemotherapy, which affects both cancer and healthy cells throughout the body, radiation therapy can be focused on specific areas, minimizing damage to surrounding healthy tissues.
In the context of liver cancer, radiation therapy may be used to:
- Shrink tumors before surgery
- Treat tumors that are inoperable due to their location or size
- Provide relief from symptoms in advanced liver cancer
There are two main types of radiation therapy used for liver cancer:
- External beam radiation therapy (EBRT): Radiation is delivered from outside the body using a machine.
- Internal radiation therapy (brachytherapy): Radioactive sources are placed inside or very close to the tumor to deliver radiation directly.
3. Indications for Radiation Therapy in Liver Cancer
Radiation therapy is not typically the first choice for liver cancer treatment, as other therapies like surgery, liver transplantation, or ablation may be more effective in certain cases. However, there are specific circumstances where radiation therapy is used, either as a primary treatment or in combination with other therapies.
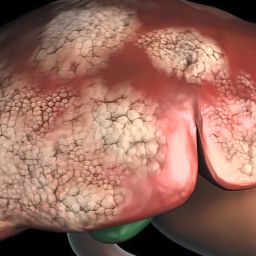
3.1 Inoperable or Unresectable Liver Tumors
One of the most common indications for radiation therapy in liver cancer is when the tumor cannot be surgically removed due to its location, size, or the patient’s overall health. Patients with advanced liver disease, such as cirrhosis, may not be suitable candidates for surgery, and in these cases, radiation therapy offers an alternative treatment option.
Radiation therapy can be used to:
- Shrink the tumor, which may help alleviate symptoms and improve quality of life.
- Prevent further tumor growth, thereby managing the disease for a longer period.
- Provide palliative care for patients who are not candidates for surgery but still require relief from symptoms such as pain or obstruction.
3.2 Radiation Therapy as a Part of Multimodal Treatment
In some cases, radiation therapy is used in combination with other treatments, such as chemotherapy, surgery, or liver transplantation. This multimodal approach can improve outcomes for patients by targeting the cancer from multiple angles.
- Pre-surgical treatment: Radiation therapy can be used before surgery to shrink a tumor, making it easier to remove and increasing the likelihood of a successful surgical outcome.
- Post-surgical treatment: In some cases, radiation therapy may be used after surgery to target any remaining cancer cells and reduce the risk of recurrence.
- Combination with chemotherapy: Radiation therapy is sometimes combined with chemotherapy, particularly when surgery is not an option. The two treatments can work together to attack cancer cells in different ways, potentially improving the effectiveness of the treatment plan.
3.3 Palliative Care for Advanced Liver Cancer
In patients with advanced-stage liver cancer or those who are not candidates for curative treatments, radiation therapy is often used as part of palliative care. Palliative radiation therapy aims to relieve symptoms, reduce tumor size, and improve the quality of life for patients.

Common uses of radiation therapy in palliative care include:
- Pain relief: Radiation therapy can be used to treat tumors that are causing pain by reducing their size and relieving pressure on surrounding tissues.
- Control of bleeding: Tumors in the liver can sometimes cause bleeding. Radiation therapy can help shrink the tumor and reduce the risk of bleeding.
- Obstruction relief: In some cases, tumors may block bile ducts or blood vessels, leading to jaundice or other complications. Radiation therapy can help alleviate such blockages.
3.4 Targeting Liver Metastasis
Liver cancer can sometimes be secondary, meaning it has spread from another part of the body, such as the colon, lungs, or breasts. When this happens, the cancer is referred to as metastatic liver cancer. In cases where liver metastases cannot be treated with surgery or other localized therapies, radiation therapy can be used to target the metastatic tumors, reduce their size, and alleviate symptoms like pain or obstruction.
While radiation therapy is not a cure for metastatic liver cancer, it can help improve symptoms and slow the progression of the disease, providing patients with better quality of life.
4. Types of Radiation Therapy Used for Liver Cancer
There are various radiation therapy techniques available for liver cancer, and the choice of which to use depends on the tumor’s size, location, and stage.
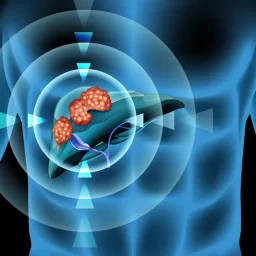
4.1 External Beam Radiation Therapy (EBRT)
External beam radiation therapy (EBRT) involves directing high-energy rays from outside the body onto the tumor. This is typically done in daily sessions over the course of several weeks. EBRT is a non-invasive procedure and can be used to treat tumors that are located in areas of the liver that are not easily accessible through surgery.
Modern techniques such as stereotactic body radiation therapy (SBRT) or stereotactic ablative radiotherapy (SABR) can deliver high doses of radiation precisely to the tumor, minimizing the impact on surrounding healthy tissues. SBRT is particularly effective for small tumors or those located in areas of the liver that are difficult to treat with other modalities.
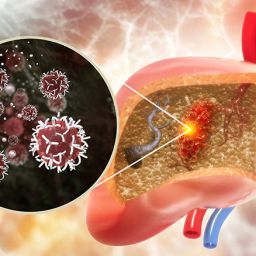
4.2 Internal Radiation Therapy (Brachytherapy)
Brachytherapy involves placing radioactive material directly inside or very close to the tumor. This method allows for higher doses of radiation to be delivered directly to the cancer cells while limiting the exposure of surrounding tissues to radiation. Brachytherapy is less commonly used for liver cancer than EBRT but can be an option for certain patients with localized tumors.
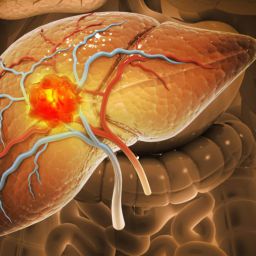
4.3 Radioembolization
Radioembolization is a type of internal radiation therapy that is used specifically for liver cancer, especially in patients with inoperable HCC or metastatic cancer. This procedure involves the injection of tiny radioactive beads into the blood vessels that supply the tumor. The beads release radiation directly to the cancerous tissue, targeting the tumor while sparing healthy liver tissue.
This treatment is often used in conjunction with other therapies, such as chemotherapy, and is considered a form of palliative treatment for patients who are not candidates for surgery.
5. Side Effects of Radiation Therapy
While radiation therapy can be effective in treating liver cancer, it is not without potential side effects. The side effects can vary depending on the type of radiation used, the location of the tumor, and the patient’s overall health.
Common side effects of radiation therapy for liver cancer include:
- Fatigue: Many patients experience fatigue during and after radiation therapy.
- Nausea and vomiting: These symptoms are common, especially if the radiation is directed toward the stomach or gastrointestinal system.
- Liver damage: Although radiation is carefully targeted, some healthy liver tissue may still be affected, potentially leading to liver dysfunction.
- Skin irritation: The skin in the area being treated may become red, dry, or irritated.
- Abdominal pain: Some patients may experience pain in the abdominal area as a result of the radiation treatment.
Side effects are generally temporary and can be managed with medication or other supportive measures. It’s important for patients to discuss potential side effects with their oncologist to understand what to expect during treatment.
Radiation therapy plays an important role in the treatment of liver cancer, particularly for patients with inoperable tumors, metastatic liver cancer, or those requiring palliative care. While it is not the first-line treatment for liver cancer, radiation therapy can provide significant benefits, including tumor shrinkage, symptom relief, and improved quality of life.
The decision to use radiation therapy depends on various factors, including the location and stage of the tumor, the patient’s overall health, and whether other treatment options are available. Advances in radiation technology, such as stereotactic radiation and radioembolization, have improved the precision and effectiveness of liver cancer treatment, offering patients more options for managing the disease.
As with any cancer treatment, radiation therapy should be considered as part of a comprehensive treatment plan that may include surgery, chemotherapy, targeted therapy, and immunotherapy. A multidisciplinary approach is often necessary to provide the best outcomes for patients with liver cancer.