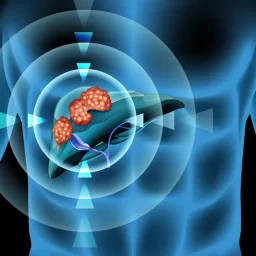
1. Chronic Liver Diseases and Cirrhosis
The presence of chronic liver diseases is one of the most significant risk factors for liver cancer. Conditions that cause long-term inflammation and liver damage greatly increase the likelihood of developing hepatocellular carcinoma.
1.1 Chronic Hepatitis B and Hepatitis C Infections
Chronic infection with hepatitis B (HBV) or hepatitis C (HCV) is a leading cause of liver cancer worldwide. Both viruses can cause persistent inflammation in the liver, which over time can lead to fibrosis, cirrhosis, and eventually liver cancer.

- Hepatitis B (HBV): Individuals infected with HBV are at a heightened risk for liver cancer. The virus integrates into the liver cells’ DNA, causing mutations and promoting cancerous cell growth. Even those with no obvious symptoms of liver disease may be at risk, as the infection often remains asymptomatic for many years. Hepatitis B vaccination has significantly reduced the risk of HBV-related liver cancer in areas where vaccination is widespread.
- Hepatitis C (HCV): Similar to HBV, chronic hepatitis C infection can cause liver damage, fibrosis, and cirrhosis. HCV has been a significant contributor to the rise in liver cancer cases, particularly in individuals who engage in high-risk behaviors such as intravenous drug use. Infected individuals may not show symptoms until the disease has progressed to cirrhosis or liver cancer.
Both hepatitis B and C can be controlled and even cured with antiviral treatments, which significantly reduce the risk of liver cancer.
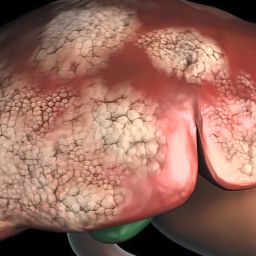
1.2 Cirrhosis
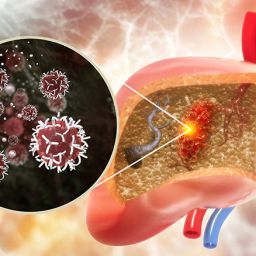
Cirrhosis is a condition characterized by the scarring of the liver tissue, which can occur as a result of chronic liver diseases such as hepatitis or excessive alcohol consumption. Over time, cirrhosis can lead to liver dysfunction, increase the risk of liver cancer, and accelerate tumor development. Cirrhosis can also result from non-alcoholic fatty liver disease (NAFLD), which is closely associated with obesity and metabolic syndrome.
Cirrhosis promotes an environment of chronic inflammation and cell turnover, which increases the likelihood of mutations in liver cells, making them prone to cancerous transformation.
2. Lifestyle and Environmental Factors
Certain lifestyle and environmental factors can increase the risk of liver cancer. Although these factors are often modifiable, they still contribute significantly to the global burden of the disease.
2.1 Alcohol Consumption
Chronic heavy drinking is one of the most significant modifiable risk factors for liver cancer. Alcohol-related liver disease (ALD) is the leading cause of cirrhosis in many countries, and long-term alcohol abuse contributes to liver damage, fibrosis, and cirrhosis. In turn, these conditions increase the risk of liver cancer.
Alcohol promotes liver cancer by creating an environment of oxidative stress and inflammation in liver cells, causing DNA damage that accumulates over time. Individuals with a history of heavy alcohol use are advised to reduce their intake to lower the risk of liver disease and cancer.
2.2 Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is increasingly recognized as one of the most common liver diseases globally. It is often associated with metabolic risk factors such as obesity, type 2 diabetes, and hypertension. When NAFLD progresses to non-alcoholic steatohepatitis (NASH), the liver becomes inflamed and damaged, which can eventually lead to cirrhosis and liver cancer.
Individuals with metabolic syndrome or obesity are particularly at risk for developing NAFLD and NASH, making it crucial to address these conditions through lifestyle modifications, such as improved diet, regular physical activity, and weight management.
2.3 Obesity and Type 2 Diabetes
Obesity is a well-established risk factor for liver disease, including NAFLD and NASH. Excess body fat, especially abdominal fat, contributes to insulin resistance, which can worsen liver inflammation and fat buildup. The link between obesity and liver cancer is mediated through metabolic changes and increased oxidative stress that accelerate liver cell damage and mutations.
Type 2 diabetes is commonly associated with obesity and has been linked to an increased risk of liver cancer, particularly when accompanied by other risk factors such as NAFLD. Managing blood sugar levels through diet, exercise, and medication can reduce the risk of developing liver cancer in individuals with diabetes.
2.4 Aflatoxin Exposure
Aflatoxins are toxic compounds produced by certain molds, commonly found in contaminated food, particularly grains and nuts stored in warm, humid environments. Aflatoxin exposure is a well-known risk factor for liver cancer, especially in regions of the world where food contamination is prevalent. The ingestion of aflatoxins can cause DNA damage in liver cells, leading to mutations that increase cancer risk.
The risk of liver cancer due to aflatoxin exposure is higher in individuals who also have chronic hepatitis B infection, as the two factors act synergistically to increase the likelihood of tumor development.
3. Genetic Factors
While environmental and lifestyle factors contribute significantly to liver cancer risk, genetics also play an important role. Some individuals are genetically predisposed to liver cancer, either through inherited conditions or genetic mutations that increase susceptibility to liver disease and cancer.
3.1 Hereditary Hemochromatosis
Hereditary hemochromatosis is a genetic disorder that leads to excessive iron accumulation in the body, including the liver. Over time, this iron buildup can cause liver damage, cirrhosis, and increase the risk of liver cancer. People with this genetic condition are often unaware of the excess iron in their bodies until symptoms appear later in life. Early detection and treatment, such as bloodletting or iron-chelating therapy, can help prevent the progression to liver cancer.
3.2 Alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin deficiency is a genetic disorder that affects the liver and lungs. The deficiency of this protein leads to the accumulation of abnormal protein in the liver, causing liver damage, cirrhosis, and an increased risk of liver cancer. Although this condition is rare, individuals with a family history of alpha-1 antitrypsin deficiency should be aware of their heightened risk.
3.3 Genetic Mutations and Liver Cancer Risk
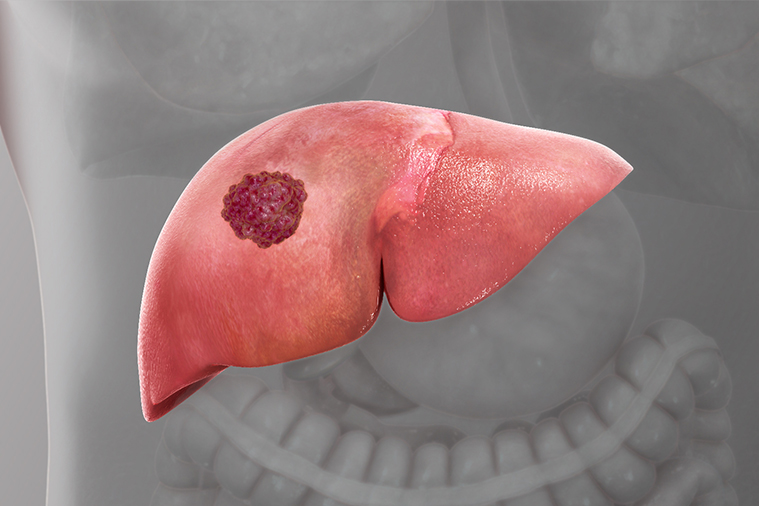
In addition to inherited genetic conditions, certain gene mutations increase an individual’s susceptibility to liver cancer. Mutations in genes such as TP53, CTNNB1, and TERT have been linked to liver cancer development, particularly in individuals with chronic liver disease or cirrhosis. These mutations can disrupt normal cell growth and repair mechanisms, allowing liver cells to become cancerous.
Genetic testing can help identify individuals with inherited genetic mutations that may predispose them to liver cancer, allowing for early surveillance and prevention strategies.
4. Age and Gender
Age and gender are non-modifiable risk factors for liver cancer. The incidence of liver cancer increases with age, particularly in individuals over 50. This is likely due to the cumulative effect of environmental exposures, chronic diseases, and genetic mutations over time.
In terms of gender, men are at a higher risk for liver cancer than women. The reasons behind this gender disparity are not fully understood, but hormonal differences, lifestyle factors, and a higher prevalence of risk factors such as alcohol consumption and hepatitis B and C infections in men may contribute.
5. Family History and Ethnicity
A family history of liver cancer can increase an individual’s risk, particularly if there is a history of liver disease or genetic predispositions such as hereditary hemochromatosis. People with a first-degree relative who has had liver cancer should discuss their risk with a healthcare provider and may require more frequent surveillance.
Ethnicity is also a factor in liver cancer risk. Certain populations are more susceptible to liver cancer due to genetic, environmental, or lifestyle factors. For instance, individuals of Asian and African descent have a higher incidence of hepatitis B infection, which significantly raises the risk of liver cancer. Similarly, people of Hispanic or Mediterranean descent may have a higher likelihood of developing liver cancer due to conditions like hereditary hemochromatosis.
6. Prevention and Early Detection
Preventing liver cancer involves addressing the modifiable risk factors such as controlling hepatitis infections, reducing alcohol consumption, maintaining a healthy weight, and managing diabetes. Vaccination against hepatitis B can prevent infection, and antiviral treatments for hepatitis C can reduce the risk of liver cancer.
Early detection is crucial for improving liver cancer survival rates. Regular screenings for individuals at high risk, including those with chronic liver disease, cirrhosis, or a family history of liver cancer, can help identify cancer at an early, more treatable stage. Surveillance methods include blood tests for liver function markers and imaging studies such as ultrasound and CT scans.
Liver cancer is a complex disease influenced by a combination of genetic, environmental, and lifestyle factors. Individuals with chronic liver diseases, viral infections, alcohol abuse, obesity, or a family history of liver cancer are at a higher risk of developing this aggressive cancer. While some risk factors are non-modifiable, many can be managed or reduced through lifestyle changes, medical interventions, and regular screenings. Identifying individuals at high risk for liver cancer is essential for early detection and prevention, offering hope for better outcomes and improved survival rates.