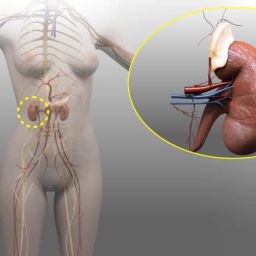
1. Radiation Therapy in the Context of Adrenal Gland Tumors
Radiation therapy (RT) uses high-energy radiation to destroy cancer cells by damaging their DNA, thereby halting their ability to grow and divide. In the case of adrenal gland tumors, RT is usually considered in specific circumstances, such as when a tumor is inoperable, when surgery carries high risks, or when the tumor has metastasized (spread to other parts of the body).
RT is also considered as a palliative measure to alleviate symptoms caused by large tumors or advanced-stage cancer. In such cases, RT may not cure the tumor but can significantly reduce tumor size, providing relief from pain and discomfort.
1.1. Indications for Radiation Therapy
The primary indications for radiation therapy in adrenal gland tumors include:
- Unresectable or Inoperable Tumors: Adrenal tumors that cannot be surgically removed due to their location, size, or involvement with nearby vital organs may be treated with radiation therapy.
- Metastatic Adrenal Tumors: Adrenal tumors that have spread to distant parts of the body may be treated with radiation therapy, either as a primary treatment or alongside systemic therapies such as chemotherapy or immunotherapy.
- Recurrent Tumors: If an adrenal tumor recurs after surgery or other treatments, radiation therapy may be used to shrink or control the growth of the tumor.
- Palliative Treatment: For patients with advanced adrenal cancer, where curative treatment is no longer possible, radiation therapy can be used to reduce tumor burden, manage symptoms, and improve the quality of life.
1.2. Types of Radiation Therapy for Adrenal Tumors
There are various forms of radiation therapy available for treating adrenal gland tumors. The choice of technique depends on the tumor’s size, location, and whether it is primary or metastatic.
- External Beam Radiation Therapy (EBRT): This is the most commonly used form of RT for adrenal tumors. EBRT involves directing high-energy rays from outside the body toward the tumor. The patient lies on a treatment table while the radiation machine is positioned to deliver targeted radiation to the tumor.
- Stereotactic Radiosurgery (SRS): This advanced form of radiation therapy delivers precisely targeted radiation to the tumor in a single or a few treatment sessions. SRS is especially useful for smaller tumors, or those located in difficult-to-reach areas.
- Brachytherapy: While not commonly used for adrenal tumors, brachytherapy involves placing a radiation source directly inside or near the tumor. This is more frequently used in other cancers but may be an option in select cases of adrenal carcinoma.
- Proton Therapy: Proton therapy, a more advanced form of radiation therapy, uses protons rather than x-rays to treat tumors. It may be considered for adrenal tumors, particularly when aiming to reduce damage to surrounding healthy tissues.
2. Effectiveness of Radiation Therapy in Adrenal Gland Tumors
The effectiveness of radiation therapy for adrenal tumors varies greatly depending on multiple factors, such as the tumor’s histological type, its location, and its stage.
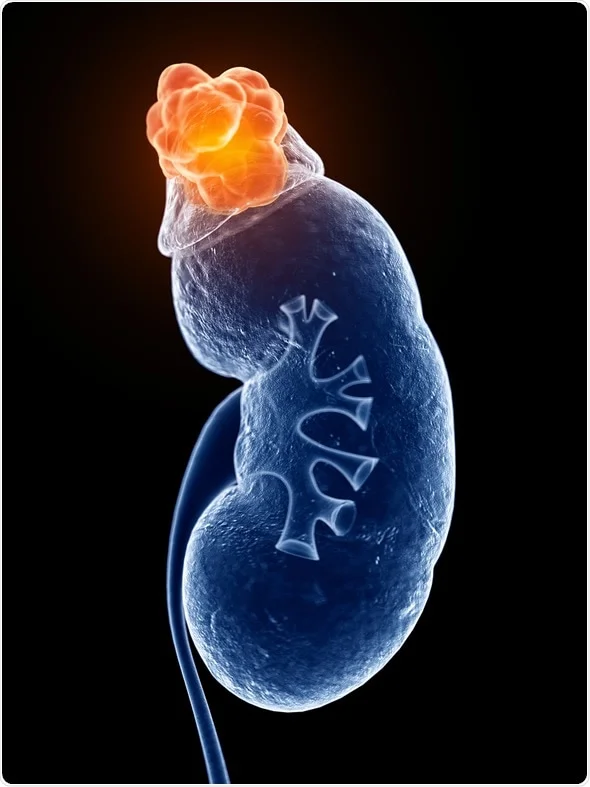
2.1. Benign vs. Malignant Tumors
For benign adrenal tumors, which include adrenal adenomas, radiation therapy is generally not the first-line treatment. Most benign tumors are small, asymptomatic, and often do not require aggressive intervention unless they become hormonally active or cause other complications.
However, in cases where a benign tumor grows or is located near vital organs, radiation may be considered to reduce its size. The effectiveness of radiation therapy in shrinking benign tumors is still an area of ongoing research and is typically seen as a supplementary treatment rather than a primary one.
In contrast, malignant tumors, such as adrenocortical carcinoma (ACC), are more likely to be treated with radiation therapy, especially in cases where surgical removal is not possible. ACC is a rare but aggressive cancer that often requires a combination of treatments. Radiation therapy in these cases has been shown to help shrink tumors, control local disease, and improve survival rates in some instances. Research suggests that while RT may not be curative, it can improve disease control when combined with other therapies.
2.2. Radiation Therapy in Metastatic Adrenal Tumors

Metastatic adrenal tumors are typically part of a broader pattern of cancer spread from other organs, such as lung cancer, breast cancer, or melanoma. When metastases to the adrenal glands occur, radiation therapy can serve a crucial role in managing these secondary tumors, particularly when the tumor is localized and cannot be surgically removed.
Radiation therapy may help to control the growth of metastatic adrenal tumors, alleviate pain, and address hormonal imbalances caused by tumor activity. However, the response to radiation can be variable, and in many cases, systemic therapies like chemotherapy or targeted treatments are more effective for controlling metastatic disease.
2.3. Effectiveness for Symptom Management
In patients with advanced adrenal cancer, especially those with large, inoperable tumors, radiation therapy may not significantly reduce the overall tumor burden but can still provide substantial benefits in symptom management. For example, RT can reduce the size of tumors that are pressing on surrounding organs, helping to alleviate symptoms such as pain, nausea, or difficulty breathing. Radiation therapy may also help control hormone secretion from tumors, reducing the adverse effects of excess hormone production (such as in Cushing’s syndrome).
3. Challenges and Limitations of Radiation Therapy
While radiation therapy has proven useful in certain contexts, it is not without its limitations. Understanding these challenges is essential when considering it as a treatment option for adrenal tumors.
3.1. Tumor Location and Size
Adrenal tumors are often located deep within the body, and large tumors may be difficult to treat with external radiation. Radiation therapy requires precision to avoid damaging surrounding tissues such as the kidneys, liver, and intestines, which are in close proximity to the adrenal glands. Larger tumors may also require higher doses of radiation, which can increase the risk of side effects.
3.2. Radiation Resistance
Some tumors, particularly advanced or highly aggressive cancers, may be resistant to radiation therapy. This can limit the effectiveness of RT as a standalone treatment. In such cases, a combination of therapies, including chemotherapy, surgery, and immunotherapy, may be necessary to achieve optimal outcomes.
3.3. Side Effects
Radiation therapy is associated with a range of potential side effects, both short-term and long-term. Short-term effects may include fatigue, skin irritation at the treatment site, nausea, and loss of appetite. Long-term effects can include tissue scarring, damage to healthy organs, and an increased risk of secondary cancers due to radiation exposure. Careful planning and advanced radiation techniques, such as stereotactic radiosurgery, can help minimize these risks.
4. Combination Therapy: Enhancing the Effectiveness of Radiation
In many cases, radiation therapy is used in conjunction with other treatment modalities to improve overall effectiveness. Combining radiation with surgery, chemotherapy, or immunotherapy can lead to better outcomes in treating adrenal tumors.
4.1. Surgery and Radiation Therapy
For patients with operable adrenal tumors, surgery remains the gold standard. However, radiation therapy may be used as an adjunctive treatment to reduce tumor size prior to surgery or to target any remaining tumor cells after surgical resection. In cases of recurrent tumors or inoperable cancers, radiation therapy may be used to prevent further tumor growth and metastasis.
4.2. Chemotherapy and Radiation Therapy
Chemotherapy is commonly used for treating advanced or metastatic adrenal tumors, particularly when surgery is not possible. Combining chemotherapy with radiation therapy can help to target the tumor from different angles, with chemotherapy working systemically and radiation focusing on localized disease.
4.3. Immunotherapy and Radiation Therapy
Emerging research has shown that combining immunotherapy with radiation may enhance the immune system’s ability to recognize and attack cancer cells. Studies are underway to assess the potential of this combination in treating adrenal tumors, particularly in metastatic cases.
5. Future Perspectives: Advancing Radiation Techniques for Adrenal Tumors
Radiation therapy continues to evolve, with new technologies improving the precision and effectiveness of treatments. For adrenal tumors, the development of more targeted radiation techniques holds promise for minimizing side effects and improving treatment outcomes.
5.1. Stereotactic Radiosurgery (SRS)
SRS is a cutting-edge technique that uses highly focused radiation beams to treat tumors with extreme precision. This approach is particularly effective for small or well-defined adrenal tumors, allowing high doses of radiation to be delivered directly to the tumor while minimizing damage to surrounding tissues.
5.2. Proton Therapy
Proton therapy is a form of radiation therapy that uses protons instead of x-rays. It offers more precise targeting, which can be particularly advantageous for tumors located near critical organs. Although still relatively new and expensive, proton therapy shows promise in improving the outcomes of adrenal tumor treatment, especially in pediatric patients and those with complex tumor locations.
Radiation therapy is an important tool in the treatment of adrenal gland tumors, particularly for tumors that are inoperable, metastatic, or recurrent. While it is not a first-line treatment, its role in providing symptom relief, controlling tumor growth, and improving patient outcomes cannot be underestimated. Ongoing advances in radiation technology and a deeper understanding of tumor biology promise to improve the efficacy and safety of radiation therapy in the future. As part of a multidisciplinary treatment approach, radiation therapy offers significant benefits to patients with adrenal gland tumors, especially when used in combination with other therapies.