1. Understanding the Impact of Chronic Pancreatitis on Digestion
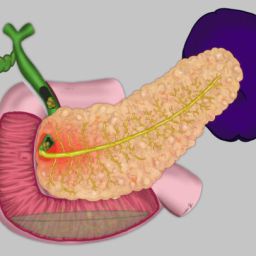
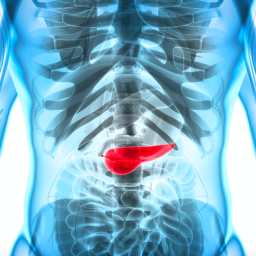
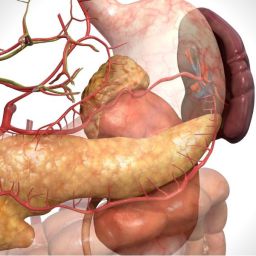
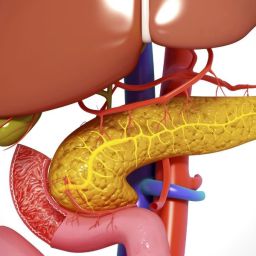
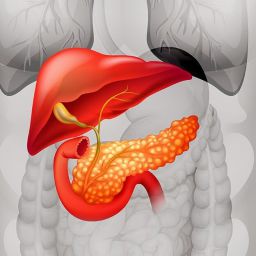
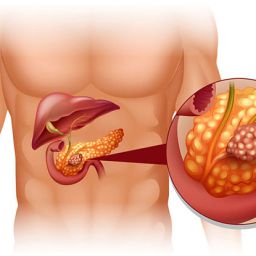
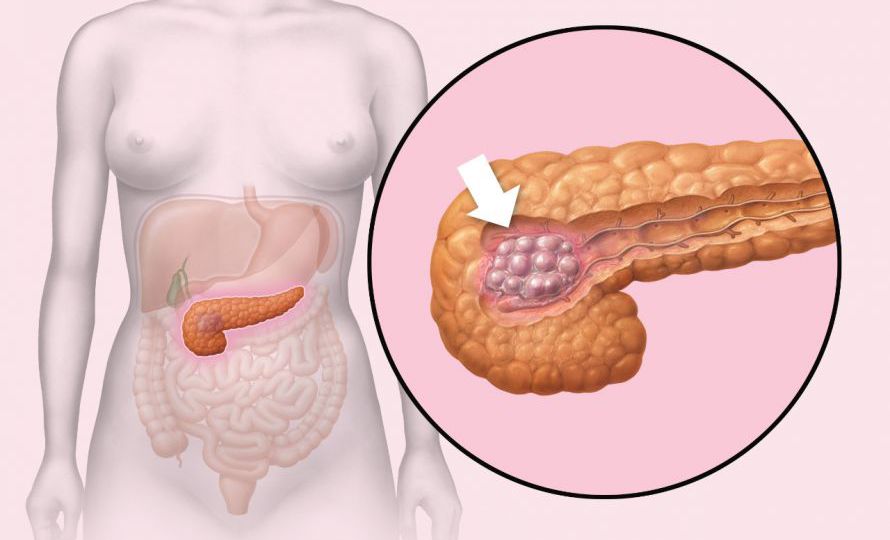
The pancreas plays a vital role in digestion by producing enzymes that break down fats, proteins, and carbohydrates, as well as hormones that regulate blood sugar levels. In chronic pancreatitis, the inflammation of the pancreas leads to the destruction of these enzymes and hormones, causing digestive difficulties.
The loss of digestive enzymes means that individuals with chronic pancreatitis may have trouble breaking down and absorbing essential nutrients from food. This can lead to malnutrition, weight loss, and vitamin deficiencies. Additionally, the pain associated with chronic pancreatitis, often triggered by eating, can make it difficult to maintain a healthy diet. Therefore, making informed dietary choices is crucial for managing symptoms and preventing further complications.
2. Foods to Include in the Diet for Chronic Pancreatitis
Certain foods are particularly beneficial for individuals with chronic pancreatitis, as they can help alleviate symptoms, improve digestion, and support overall pancreatic health. Here are the key food groups and specific foods that should be prioritized:
a. Lean Proteins
Proteins are essential for repairing tissue and maintaining muscle mass, but they need to be consumed in easily digestible forms for individuals with chronic pancreatitis. Lean protein sources are ideal because they are lower in fat and less likely to trigger inflammation.

- Recommended Lean Proteins:
- Skinless poultry (chicken, turkey)
- Fish (preferably fatty fish like salmon, trout, and sardines)
- Egg whites
- Tofu and tempeh
- Low-fat dairy products (such as Greek yogurt and cottage cheese)
These lean proteins are not only easy on the digestive system but also provide essential amino acids necessary for healing and maintaining body functions.
b. Low-Fat Foods
Because individuals with chronic pancreatitis may have difficulty digesting fats, consuming low-fat foods is crucial to reducing stress on the pancreas. High-fat foods can worsen symptoms like abdominal pain, bloating, and diarrhea, making it important to focus on foods with a minimal fat content.
- Low-Fat Food Choices:
- Fruits and vegetables (low in fat and high in fiber)
- Whole grains like oats, brown rice, and quinoa
- Legumes and lentils (rich in fiber and protein)
- Non-fat or low-fat dairy products
- Lean cuts of meat and fish
A low-fat diet reduces the burden on the pancreas and promotes better digestion, helping to prevent inflammation and discomfort.
c. Fiber-Rich Foods
Fiber is an important nutrient for digestive health, as it helps regulate bowel movements and prevents constipation. For individuals with chronic pancreatitis, fiber-rich foods can support gut health by improving digestion and reducing the likelihood of diarrhea or bloating.
- High-Fiber Foods to Include:
- Whole grains (brown rice, oats, barley)
- Vegetables (especially leafy greens like spinach, kale, and broccoli)
- Fruits (apples, pears, and berries)
- Legumes (beans, lentils, chickpeas)
- Nuts and seeds (in moderation)
Fiber is beneficial for managing digestive symptoms, and it can also help control blood sugar levels, which is important for individuals at risk of developing diabetes, a common complication of chronic pancreatitis.
d. Antioxidant-Rich Foods
Antioxidants play a vital role in reducing inflammation and protecting the body from oxidative stress. Chronic pancreatitis often leads to systemic inflammation, and consuming foods rich in antioxidants can help mitigate this effect, supporting both pancreatic and overall health.

- Recommended Antioxidant-Rich Foods:
- Berries (blueberries, strawberries, raspberries)
- Dark leafy greens (spinach, kale)
- Nuts (almonds, walnuts)
- Tomatoes and bell peppers
- Carrots and sweet potatoes
These foods can help lower inflammation, support immune function, and improve general health, making them important additions to the diet of individuals with chronic pancreatitis.
3. Foods to Avoid in Chronic Pancreatitis
While some foods can support health, others can exacerbate the symptoms of chronic pancreatitis and should be limited or avoided. The following foods should be carefully managed in the diet to prevent triggering flare-ups or increasing inflammation:
a. High-Fat Foods
Fatty foods put the pancreas under extra strain because the pancreas must release digestive enzymes to break down fat. In individuals with chronic pancreatitis, the pancreas may not produce enough enzymes, making it difficult to digest fat and increasing the risk of pain and discomfort.
- Foods to Avoid:
- Fried foods (such as french fries, fried chicken)
- Fatty cuts of meat (such as bacon, sausage, and fatty steaks)
- Full-fat dairy products (cream, butter, cheese)
- Fast food or processed snacks (chips, pastries, etc.)
To reduce pancreatic stress and minimize discomfort, it is crucial to limit fat intake and choose low-fat or fat-free alternatives.
b. Alcohol
Alcohol is one of the primary risk factors for developing chronic pancreatitis, and it can also trigger flare-ups in individuals who already have the condition. Alcohol consumption exacerbates inflammation, impairs pancreatic function, and increases the risk of further complications. For this reason, it is strongly advised that individuals with chronic pancreatitis completely avoid alcohol.
4. Creating a Balanced Diet Plan for Chronic Pancreatitis
When managing chronic pancreatitis, a balanced diet plan is essential to minimize symptoms, support pancreatic function, and prevent malnutrition. Here are some tips to help create a diet plan tailored to the needs of individuals with chronic pancreatitis:
- Meal Frequency: Small, frequent meals throughout the day can help reduce the workload on the pancreas and improve digestion. This approach also helps prevent large, burdensome meals that could trigger discomfort.
- Avoid Overeating: Eating in moderation is key, as consuming large portions may strain the digestive system and worsen symptoms.
- Supplements: Since chronic pancreatitis may impair nutrient absorption, individuals may require vitamin and mineral supplements, such as fat-soluble vitamins (A, D, E, and K) and pancreatic enzyme replacements, to support digestion.
Consulting with a healthcare provider or a dietitian can help create a personalized eating plan that meets individual nutritional needs and addresses specific symptoms.
Diet plays a pivotal role in managing chronic pancreatitis and alleviating symptoms. By focusing on lean proteins, low-fat foods, fiber-rich options, and antioxidant-rich fruits and vegetables, individuals can support their digestive health and improve their overall well-being. On the other hand, it is essential to avoid high-fat foods, alcohol, refined sugars, and irritating foods, as they can trigger flare-ups and worsen the condition.
Creating a balanced and sustainable diet plan tailored to individual needs can help individuals with chronic pancreatitis manage their condition effectively, reduce stress on the pancreas, and enhance their quality of life.