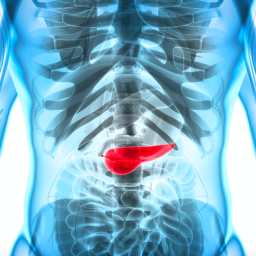
1. Clinical Evaluation and Medical History
The initial step in diagnosing IPMN often begins with a detailed medical history and clinical evaluation. While imaging and laboratory tests play a significant role in the diagnosis, understanding the patient’s symptoms, risk factors, and medical background is essential.
Symptoms of IPMN
The symptoms of IPMN can vary depending on the size, location, and type of IPMN. Some of the common symptoms include:
- Abdominal pain
- Weight loss
- Jaundice (yellowing of the skin and eyes)
- Nausea and vomiting
- Pancreatitis
If these symptoms are present, especially in individuals with a history of pancreatic conditions, doctors may suspect the presence of an IPMN and proceed with further diagnostic testing.
Risk Factors
Several factors can increase the likelihood of developing IPMN:
- Family history of pancreatic cancer
- Genetic mutations (e.g., mutations in the cystic fibrosis gene)
- Age (IPMN is more common in people over 50)
- Chronic pancreatitis
A thorough medical history and awareness of these risk factors can help clinicians decide on the next steps for diagnosis.
2. Serum Tumor Markers
Serum tumor markers are blood tests that help detect substances produced by cancer cells or other abnormal tissues. Although not definitive for diagnosing IPMN, certain tumor markers can provide useful information about the likelihood of malignancy.
CA 19-9

The carbohydrate antigen 19-9 (CA 19-9) is one of the most commonly used tumor markers for pancreatic conditions. Elevated levels of CA 19-9 in the blood can be associated with pancreatic cancer, including IPMN with malignant transformation. However, CA 19-9 is not specific to IPMN and can also be elevated in conditions like pancreatitis, liver disease, and other cancers.
CEA (Carcinoembryonic Antigen)
Carcinoembryonic antigen (CEA) is another tumor marker that can be elevated in IPMN, particularly when there is evidence of malignancy. Like CA 19-9, CEA is not specific to IPMN and can also be elevated in other gastrointestinal cancers.
Limitations of Tumor Markers While useful in monitoring progression, serum tumor markers should not be relied upon as a sole diagnostic tool. They are often used in conjunction with imaging and clinical findings.
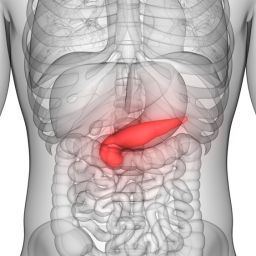
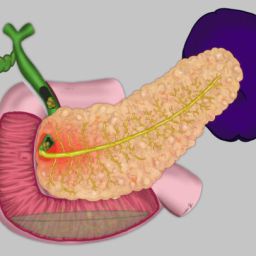
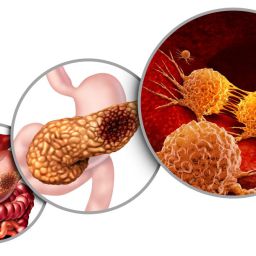
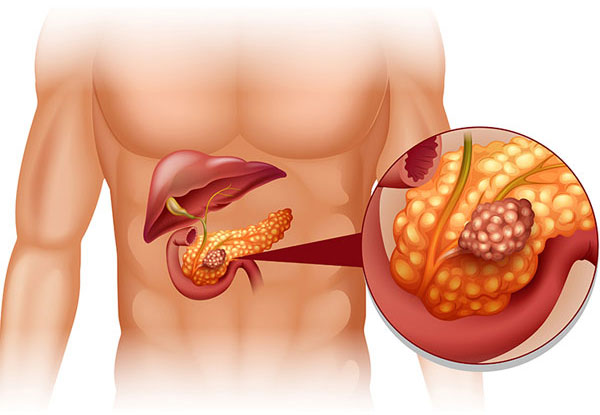
3. Imaging Methods
Imaging plays a pivotal role in diagnosing IPMN. It allows doctors to visualize the pancreatic ducts and any cystic lesions that may be present. The most common imaging methods include:
3.1. Ultrasound (US)
Ultrasound is often the first imaging modality used to identify potential pancreatic abnormalities. It is non-invasive, widely available, and relatively inexpensive.
- Usefulness: Ultrasound can detect cystic lesions in the pancreas, but it is less effective in visualizing deeper structures due to the gas in the bowel. It is most useful in detecting larger cysts and can help guide further testing.
- Limitations: It is not as effective in evaluating smaller lesions or assessing the pancreatic ducts in detail. Therefore, if abnormalities are detected, additional imaging techniques will be required.
3.2. Computed Tomography (CT) Scan
CT imaging is a more advanced imaging modality used to assess IPMN and other pancreatic disorders. It provides high-resolution images of the pancreas and surrounding tissues, which can help detect the presence of cysts, ductal dilation, and other abnormalities.
- Usefulness: CT scans are highly effective in detecting pancreatic cysts, especially in larger tumors. They can also provide detailed information on the size, location, and features of the cystic lesions. CT can also help assess whether there is evidence of malignancy, such as irregular cyst walls, solid components, or lymph node involvement.
- Limitations: A CT scan is not the best for evaluating the ductal system in detail, and radiation exposure is a concern with repeated imaging.
3.3. Magnetic Resonance Imaging (MRI) and MRCP
Magnetic Resonance Imaging (MRI) and Magnetic Resonance Cholangiopancreatography (MRCP) are non-invasive imaging techniques that provide detailed images of the pancreas, biliary tree, and pancreatic ducts.
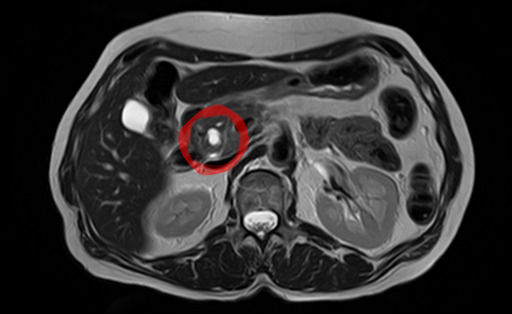
- Usefulness: MRCP is particularly useful in visualizing the pancreatic ducts, detecting ductal dilatation, and identifying cystic lesions within the ducts. MRI can also evaluate the structure of the cysts and detect any signs of malignancy. MRCP, in particular, is considered the gold standard for imaging the pancreatic duct system.
- Advantages: MRI/MRCP can provide highly detailed images without the use of radiation, making it safer for repeated assessments. It is also useful in detecting smaller cysts and evaluating the extent of the disease.
- Limitations: MRI/MRCP may not be as widely available as other imaging techniques and may require more time to obtain high-quality images.
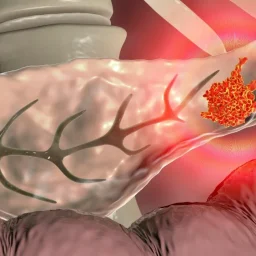
3.4. Endoscopic Ultrasound (EUS)
Endoscopic Ultrasound (EUS) is a highly sensitive imaging technique that combines endoscopy with ultrasound to provide detailed images of the pancreas and surrounding tissues.
- Usefulness: EUS is considered one of the most effective methods for evaluating pancreatic cysts, including IPMN. It allows for high-resolution imaging and can provide information about the cyst’s characteristics, including size, location, and internal features. Additionally, EUS can be used to perform fine needle aspiration (FNA) for cytological analysis of cyst fluid, which is crucial for determining the risk of malignancy.
- Advantages: EUS is highly sensitive and can detect small cysts that may not be visible with other imaging methods. It also allows for tissue sampling, which can be essential for determining the malignancy risk.
- Limitations: EUS is invasive, requiring the insertion of an endoscope into the stomach or duodenum, and is typically performed under sedation. While it is highly accurate, it is more expensive and less readily available than non-invasive imaging methods.
4. Endoscopic Retrograde Cholangiopancreatography (ERCP)
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a specialized technique that combines endoscopy with X-ray to visualize the pancreatic and bile ducts. It is less commonly used in the initial diagnosis of IPMN but may be necessary for therapeutic interventions or when other imaging methods are inconclusive.
- Usefulness: ERCP can provide detailed images of the pancreatic duct system, allowing for the assessment of any blockages, strictures, or cysts within the ducts. It can also be used to obtain samples of ductal tissue for biopsy.
- Limitations: ERCP is invasive and carries risks, such as pancreatitis, bleeding, and infection. It is not typically used as a first-line diagnostic tool for IPMN but may be employed in specific cases.
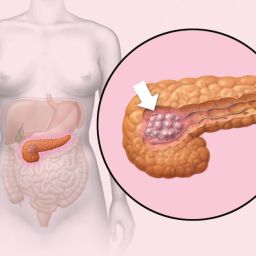
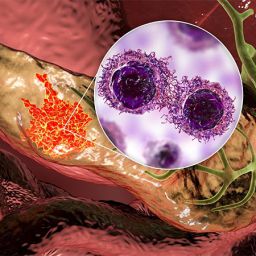
5. Biopsy and Cytological Analysis
Although imaging plays a significant role in diagnosing IPMN, definitive diagnosis and risk assessment often require a biopsy. A biopsy can be performed through techniques like EUS-guided fine needle aspiration (FNA) to obtain cyst fluid.
- Usefulness: Cytological analysis of cyst fluid can help determine the type of IPMN and assess the risk of malignancy. The fluid may be tested for molecular markers, such as KRAS mutations, which can provide additional insights into the behavior of the neoplasm.
- Limitations: Obtaining an adequate sample for biopsy may be challenging, especially for smaller cysts or lesions in difficult-to-reach areas of the pancreas.
6. Genetic Testing
Genetic testing is emerging as an important tool in the diagnosis of IPMN, particularly in patients with a family history of pancreatic cancer or other genetic predispositions.
- Usefulness: Genetic testing can help identify specific mutations that increase the risk of developing IPMN and other pancreatic diseases. For example, mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene can predispose individuals to the development of IPMN.
- Limitations: Genetic testing is not routinely used for diagnosing IPMN, but it may be considered for individuals with a strong family history of pancreatic cancer or hereditary cancer syndromes.
Diagnosing IPMN requires a multifaceted approach involving clinical evaluation, laboratory tests, imaging studies, and sometimes biopsy. Each method provides crucial information that helps determine the presence of IPMN, the extent of the disease, and the risk of malignancy. The combination of non-invasive imaging techniques like MRCP and EUS, along with serum markers and genetic testing, offers a comprehensive diagnostic strategy that can guide treatment decisions and patient management. Early detection and accurate diagnosis are vital for improving the prognosis and outcomes for individuals with IPMN.