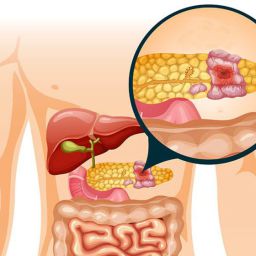
1. Stage of the Cancer at Diagnosis
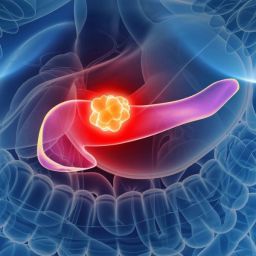
The stage at which pancreatic cancer is diagnosed is one of the most significant determinants of the patient’s prognosis. Pancreatic cancer is often diagnosed at an advanced stage when the tumor has already spread to other parts of the body, making it more difficult to treat effectively.
1.1 Localized vs. Metastatic Pancreatic Cancer
- Localized Pancreatic Cancer: When the cancer is confined to the pancreas and has not spread to surrounding tissues or distant organs, the prognosis is better. Surgical removal of the tumor may be possible, and the patient may have a chance of long-term survival.
- Metastatic Pancreatic Cancer: When the cancer has spread to other organs, such as the liver, lungs, or peritoneum, the prognosis becomes significantly worse. Metastasis limits treatment options, and the focus shifts to managing symptoms and improving the patient’s quality of life.
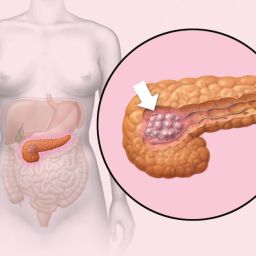
1.2 Resectability of the Tumor
A major factor in determining the prognosis is whether the tumor is resectable, meaning it can be surgically removed. In cases where the tumor is small, localized, and has not spread to nearby blood vessels or lymph nodes, surgery may be an option, offering the best chance for a cure. However, pancreatic tumors are often diagnosed after they have grown large or have spread to nearby structures, which limits the surgical options.
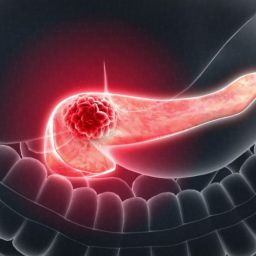
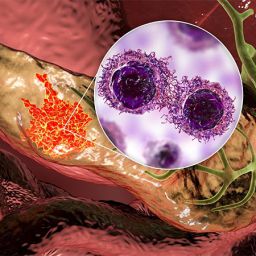
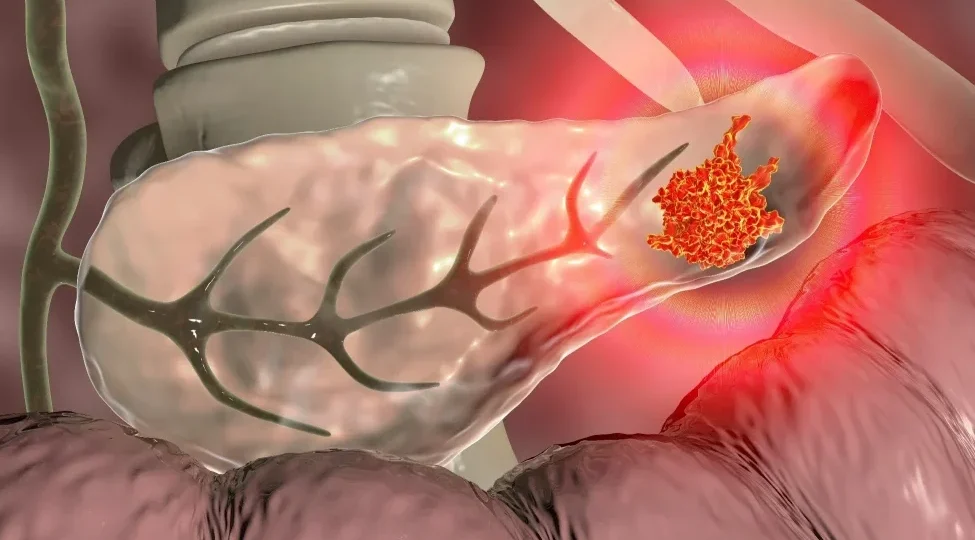
2. Tumor Characteristics and Biology
The biological behavior and molecular features of the pancreatic cancer tumor play a significant role in determining prognosis. These characteristics can influence how aggressive the cancer is, its growth rate, and its potential to respond to treatment.

2.1 Tumor Grade
Tumor grade refers to how abnormal the cancer cells look under a microscope. Low-grade tumors tend to grow slowly and have a better prognosis, whereas high-grade tumors are more aggressive, grow faster, and have a poorer prognosis. High-grade tumors are more likely to spread quickly to other parts of the body.
2.2 Tumor Size
The size of the pancreatic tumor is another key prognostic factor. Smaller tumors are easier to treat and have a better chance of being surgically removed. Larger tumors, especially those that involve nearby blood vessels or lymph nodes, are more challenging to treat and often indicate a more advanced stage of cancer.
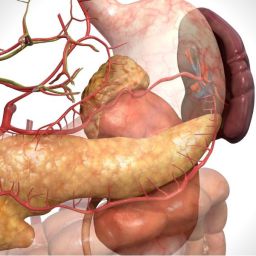
3. Surgical and Treatment Options
Treatment options significantly impact the prognosis of pancreatic cancer patients. The availability and effectiveness of surgery, chemotherapy, radiation therapy, and newer treatments such as immunotherapy and targeted therapies play a key role in survival outcomes.
3.1 Surgery
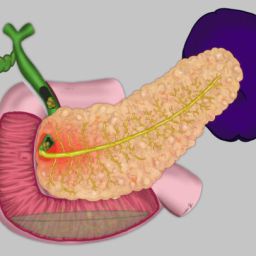
Surgical intervention is the most effective treatment for pancreatic cancer, but it is only possible if the tumor is localized and resectable. The most common surgical procedures for pancreatic cancer are:
- Whipple Procedure (Pancreaticoduodenectomy): This is the most common surgery for tumors located in the head of the pancreas. It involves the removal of the head of the pancreas, part of the small intestine, the gallbladder, and sometimes part of the stomach.
- Distal Pancreatectomy: This procedure is used for tumors in the body or tail of the pancreas, where the tail and part of the pancreas are removed.
- Total Pancreatectomy: In rare cases, the entire pancreas may be removed if the cancer is widespread within the organ.
The success of surgery depends largely on the tumor’s resectability and the patient’s overall health, including their ability to tolerate major surgery.
3.2 Chemotherapy
Chemotherapy is commonly used to treat pancreatic cancer, either as a primary treatment or as adjuvant therapy following surgery. Chemotherapy can help shrink tumors, reduce symptoms, and improve survival, but it is often not curative in cases of metastatic disease.
The most commonly used chemotherapy regimens for pancreatic cancer include FOLFIRINOX (a combination of four chemotherapy drugs) and Gemcitabine (a single chemotherapy drug). Newer combinations and more targeted therapies are currently under investigation.
3.3 Radiation Therapy
Radiation therapy uses high-energy radiation to kill cancer cells. It may be used to shrink a tumor before surgery or to relieve symptoms in advanced stages of the disease. However, pancreatic cancer is generally less responsive to radiation than other types of cancer.
4. Patient’s Overall Health and Age
The patient’s age, general health, and fitness level also play a role in determining prognosis. Younger, healthier patients may have a better chance of surviving pancreatic cancer due to their ability to tolerate aggressive treatments, such as surgery, chemotherapy, and radiation. Patients with fewer comorbidities (e.g., diabetes, heart disease) generally have better outcomes.
4.1 Performance Status
The Eastern Cooperative Oncology Group (ECOG) performance status is a scale used by doctors to measure a patient’s level of functioning. A higher performance status (indicating better overall health) is associated with better treatment outcomes and survival. Patients with a performance status of 0 or 1 are more likely to benefit from aggressive treatments, including surgery.
4.2 Nutritional Status
Malnutrition and weight loss are common in pancreatic cancer patients, particularly those with advanced disease. Poor nutritional status can impair the body’s ability to tolerate treatment and recover from surgery. Nutritional support and weight management are important in improving a patient’s prognosis and overall well-being.
5. Response to Treatment
How well a patient responds to initial treatment also plays a crucial role in determining their prognosis. Patients who show a good response to chemotherapy or surgery may have a better chance of long-term survival. In contrast, patients whose cancer recurs or spreads quickly after treatment tend to have a poorer prognosis.
5.1 Recurrence
Pancreatic cancer has a high recurrence rate, even after surgery. Recurrence typically occurs within the first few years following treatment, often in the form of metastases. Regular monitoring and follow-up scans are necessary to detect recurrence early and adjust the treatment plan accordingly.
5.2 New Treatment Approaches
As research into pancreatic cancer progresses, new treatment approaches, including personalized medicine, immunotherapy, and targeted therapies, offer hope for improving prognosis. Clinical trials continue to explore these cutting-edge therapies and their potential benefits for patients with pancreatic cancer.
Pancreatic cancer remains one of the most difficult cancers to treat, but understanding the factors that influence its prognosis can help patients and their families better navigate the treatment journey. The stage of cancer, tumor characteristics, the patient’s overall health, and their response to treatment all play crucial roles in determining outcomes.
Though the prognosis for pancreatic cancer is often poor, advancements in medical research, including new surgical techniques, chemotherapy regimens, and immunotherapies, are helping improve survival rates and quality of life for many patients. Early detection and personalized treatment approaches continue to be key in improving the outlook for patients with this challenging disease.