Challenges of Treating Pancreatic Cancer
Pancreatic cancer presents several challenges that make it difficult to treat effectively. Some of the key challenges include:
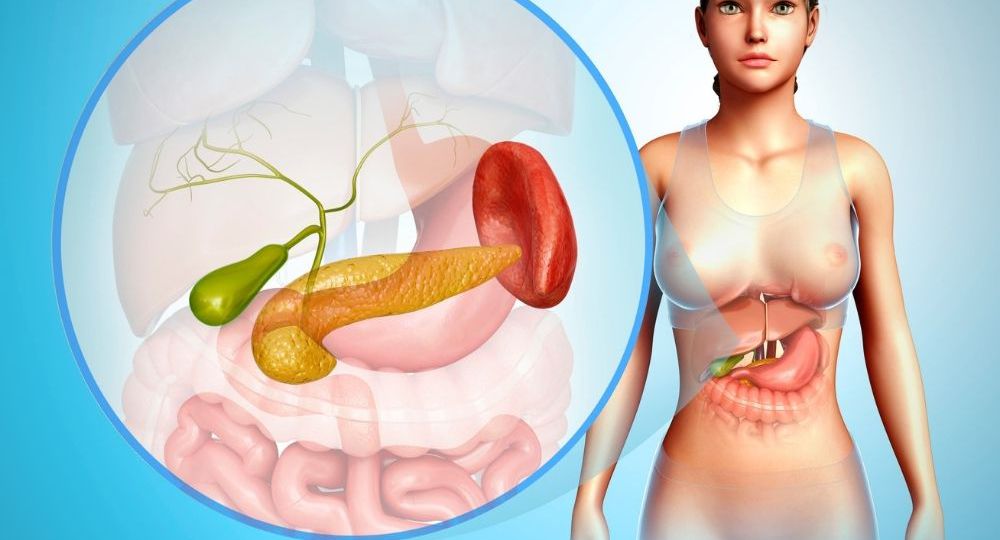
1.1. Late Diagnosis
Pancreatic cancer is notoriously difficult to detect in its early stages because it often doesn’t present noticeable symptoms until the cancer has already spread. By the time many patients are diagnosed, the cancer is already in an advanced stage, which limits treatment options and reduces the effectiveness of surgery and other treatments.
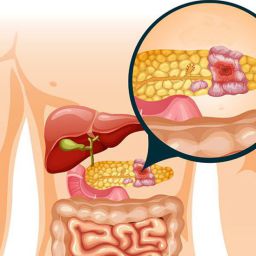
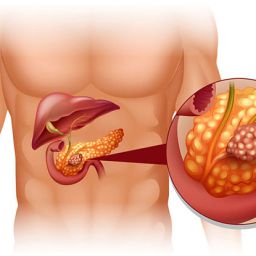
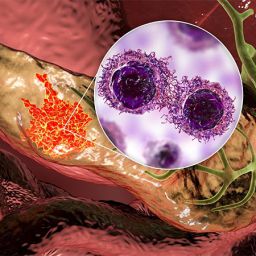
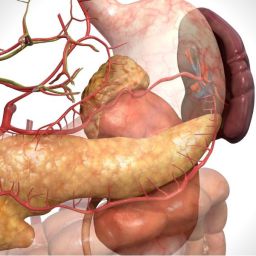
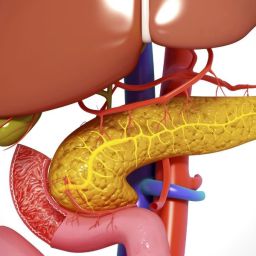
1.2. Tumor Microenvironment
The pancreas tumor microenvironment is another challenge. Pancreatic tumors tend to develop a dense stroma—a fibrous tissue surrounding the cancer cells—which can prevent chemotherapy drugs and immune cells from reaching the tumor. This “protective” barrier makes it difficult for therapies, including immunotherapy, to penetrate the tumor and effectively target the cancer cells.
1.3. Immunosuppressive Nature of Pancreatic Cancer
Unlike other cancers, pancreatic tumors tend to suppress the body’s immune response. This makes it harder for immunotherapies to activate the immune system and stimulate it to fight cancer. The presence of immunosuppressive molecules and the inability of immune cells to infiltrate the tumor contribute to the poor response to immunotherapy in pancreatic cancer patients.
2. Immunotherapy in Pancreatic Cancer: Current Approaches
While the use of immunotherapy in pancreatic cancer is still in the early stages, several approaches are being investigated. The main types of immunotherapy treatments being explored for pancreatic cancer include:
2.1. Checkpoint Inhibitors
Checkpoint inhibitors are a type of immunotherapy that block the proteins that prevent immune cells from attacking cancer cells. These proteins, known as immune checkpoints, are often exploited by cancer cells to evade the immune system.
In pancreatic cancer, immune checkpoint inhibitors have been a promising area of research. The two main checkpoint inhibitors that have shown promise in clinical trials are PD-1 inhibitors and CTLA-4 inhibitors. These drugs work by blocking the PD-1 protein on immune cells, which is often overexpressed in tumors and prevents the immune system from recognizing and attacking cancer cells.
Some of the most well-known PD-1 inhibitors include nivolumab (Opdivo) and pembrolizumab (Keytruda). While these drugs have shown remarkable efficacy in treating cancers like melanoma and non-small cell lung cancer, their effectiveness in pancreatic cancer has been more limited.
One of the key challenges in using checkpoint inhibitors for pancreatic cancer is that the tumor microenvironment tends to suppress the immune response. However, ongoing research is looking into ways to enhance the effectiveness of checkpoint inhibitors by combining them with other treatments like chemotherapy or radiation therapy.
2.2. Cancer Vaccines
Cancer vaccines are another promising immunotherapy approach. Unlike traditional vaccines that prevent infection, cancer vaccines aim to stimulate the immune system to attack existing cancer cells. In the case of pancreatic cancer, several cancer vaccines are in clinical trials, including GVAX and Cvac.
GVAX is a vaccine that contains pancreatic cancer cells that have been genetically modified to make them more visible to the immune system. Cvac, on the other hand, is an autologous vaccine made from a patient’s own tumor cells. Both vaccines are designed to stimulate the immune system to attack pancreatic cancer cells more effectively.
While these vaccines have shown some promise in early-stage trials, they are still being tested for their efficacy and safety in larger patient populations.
2.3. Monoclonal Antibodies
Monoclonal antibodies are laboratory-produced molecules that can be designed to target specific proteins found on the surface of cancer cells. In pancreatic cancer, monoclonal antibodies are being developed to target proteins like EGFR (epidermal growth factor receptor) and HER2, which are overexpressed in some pancreatic tumors.
One of the most well-known monoclonal antibodies used in the treatment of pancreatic cancer is trastuzumab (Herceptin), which targets the HER2 protein. However, it is only effective in a small subset of pancreatic cancer patients whose tumors express high levels of HER2.
Other monoclonal antibodies are being studied in combination with other therapies, including chemotherapy and immunotherapy, to enhance their efficacy and overcome the tumor’s resistance mechanisms.
2.4. Adoptive Cell Transfer and CAR-T Therapy
Adoptive cell transfer (ACT) and chimeric antigen receptor T-cell (CAR-T) therapy are advanced immunotherapy techniques that involve modifying a patient’s own immune cells to better target cancer. In CAR-T therapy, T-cells are extracted from a patient’s blood, genetically modified in a laboratory to express a receptor that can specifically target cancer cells, and then re-infused into the patient’s bloodstream.
While CAR-T therapy has shown impressive results in certain cancers like leukemia and lymphoma, its application in solid tumors like pancreatic cancer has been challenging. The dense tumor stroma and the immunosuppressive microenvironment of pancreatic cancer create significant barriers for the success of CAR-T therapy. However, researchers are exploring ways to improve CAR-T therapy’s ability to penetrate pancreatic tumors and overcome these obstacles.
3. Challenges and Limitations of Immunotherapy for Pancreatic Cancer
Despite the potential of immunotherapy for treating pancreatic cancer, several obstacles remain:

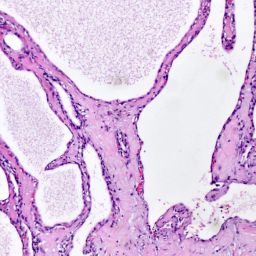
3.1. Tumor Heterogeneity
Pancreatic cancer is highly heterogeneous, meaning that the tumor can have different genetic and molecular characteristics even within the same patient. This heterogeneity makes it difficult to develop a single immunotherapy approach that will work for all patients.
3.2. Immunosuppressive Tumor Microenvironment
As mentioned earlier, the pancreatic tumor microenvironment is extremely immunosuppressive, which limits the ability of immune cells to infiltrate and target the cancer. Researchers are exploring ways to modify the tumor microenvironment to make it more receptive to immune therapies.
3.3. Limited Patient Response
While immunotherapies like checkpoint inhibitors have shown success in other cancers, their effectiveness in pancreatic cancer has been limited. Many patients with pancreatic cancer do not respond to immunotherapy, and it is unclear why some patients respond while others do not.
3.4. Side Effects and Toxicity
Like all treatments, immunotherapy can have side effects. These can range from mild symptoms such as fatigue and skin rashes to more severe immune-related adverse events, where the immune system attacks healthy tissues. Managing these side effects is crucial for ensuring the safety and effectiveness of immunotherapy in pancreatic cancer patients.
4. Recent Clinical Trials and Research
Several ongoing clinical trials are investigating the role of immunotherapy in pancreatic cancer. These trials are testing new combinations of immunotherapy with other treatments, such as chemotherapy, targeted therapy, and radiation, to enhance their effectiveness.
For instance, some trials are combining PD-1 inhibitors with chemotherapy to see if the chemotherapy can help break down the tumor’s protective barrier and allow the immune system to better target the cancer. Other trials are testing the effectiveness of vaccines in combination with immune checkpoint inhibitors to boost the body’s immune response.
The results of these trials are still in the early stages, but they offer hope for better treatment options in the future.
While immunotherapy for pancreatic cancer is still in the experimental stage, it holds promise as a potential treatment option. The unique challenges of treating pancreatic cancer, including its late diagnosis, dense tumor microenvironment, and immunosuppressive nature, make it a difficult cancer to treat. However, research into immunotherapy is progressing rapidly, and clinical trials are exploring a variety of approaches to enhance its effectiveness.
Immunotherapy could become an essential component of pancreatic cancer treatment, particularly when used in combination with other therapies like chemotherapy or radiation. While it may not be a cure for all patients, it offers hope for improving outcomes and providing a better quality of life for those affected by this deadly disease.
As research continues, it’s important for patients and healthcare providers to stay informed about the latest advancements in immunotherapy and to consider all available treatment options when managing pancreatic cancer.