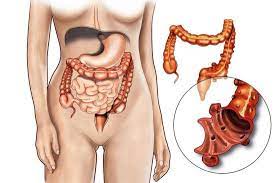
Symptoms of Sigmoid Diverticulitis
Before diving into the diagnostic methods, it’s essential to understand the symptoms of sigmoid diverticulitis. The hallmark signs of the condition include:
- Abdominal pain: Typically, the pain is located in the lower left side of the abdomen, but it can also occur in the central abdomen or radiate to the back.
- Fever: A low-grade fever may develop as the body responds to inflammation or infection.
- Changes in bowel movements: This can include diarrhea, constipation, or the presence of blood in the stool.
- Nausea and vomiting: As the condition progresses, these symptoms may occur, especially if there is an abscess or bowel obstruction.
- Bloating and gas: Some patients may experience bloating, gas, and a feeling of fullness in the abdomen.
Because many of these symptoms overlap with other gastrointestinal conditions, such as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), accurate diagnostic testing is necessary to confirm the diagnosis of sigmoid diverticulitis.
2. Initial Assessment and Clinical Examination
The diagnostic process for sigmoid diverticulitis usually begins with a thorough clinical evaluation. A healthcare provider will ask the patient about their symptoms, medical history, and risk factors. The doctor will also perform a physical examination to check for signs of tenderness, distention, and possible peritonitis (inflammation of the abdominal lining), which could indicate a more severe complication.
The physical exam might reveal:
- Tenderness in the lower left abdomen (the typical site for sigmoid diverticulitis)
- Rebound tenderness (a sign of peritoneal irritation)
- Abdominal distension or rigidity in more severe cases
While these signs suggest sigmoid diverticulitis, they are not definitive on their own, and further diagnostic tests are required to confirm the diagnosis.
3. Imaging and Diagnostic Tests for Sigmoid Diverticulitis
Once the clinical evaluation is completed, several imaging and diagnostic tests are used to confirm the diagnosis of sigmoid diverticulitis and assess its severity. These tests help differentiate diverticulitis from other conditions that may present with similar symptoms.
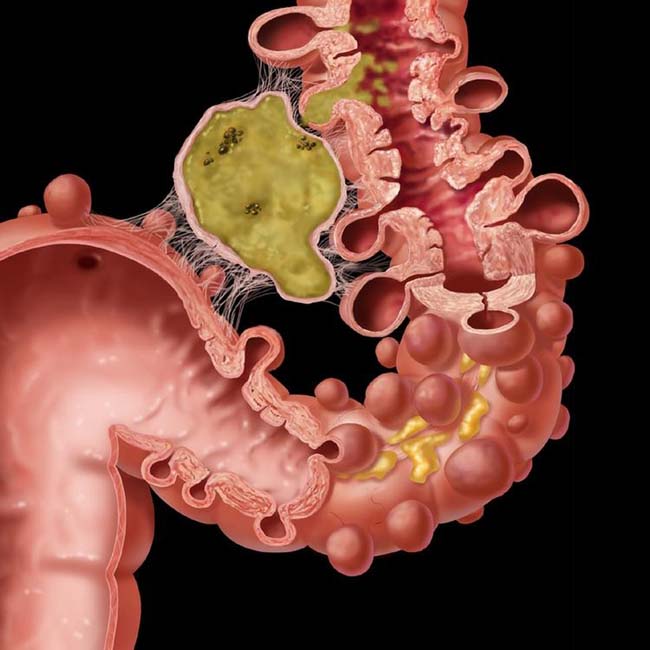
3.1. CT Scan (Computed Tomography)
The CT scan is the gold standard for diagnosing sigmoid diverticulitis. It provides detailed images of the colon and surrounding structures, allowing healthcare providers to identify the presence of inflamed diverticula, as well as complications such as abscesses, perforations, or bowel obstruction.
A CT scan can help:
- Confirm the diagnosis of diverticulitis by showing thickened colon walls, inflammation around the diverticula, and fat stranding (infiltration of fat around the inflamed area).
- Identify complications like abscess formation, perforation, or free air in the abdomen (suggesting a bowel perforation).
- Help assess the severity of the condition, guiding treatment decisions.
Typically, a contrast-enhanced CT scan is used to provide more detailed images. This test can be performed quickly and provides critical information for the treatment plan, making it the most commonly used diagnostic tool for sigmoid diverticulitis.
3.2. Ultrasound
An abdominal ultrasound is another imaging option used in the diagnosis of sigmoid diverticulitis. While less detailed than a CT scan, ultrasound can still reveal signs of diverticulitis, such as:
- Thickening of the colon wall
- Presence of diverticula
- Evidence of abscess formation or fluid collection in the abdomen
Ultrasound is non-invasive and does not involve radiation, making it a safer option for some patients, particularly those who are pregnant. However, its sensitivity and specificity are lower than CT scans, and it may not be suitable for assessing severe or complicated cases of diverticulitis.
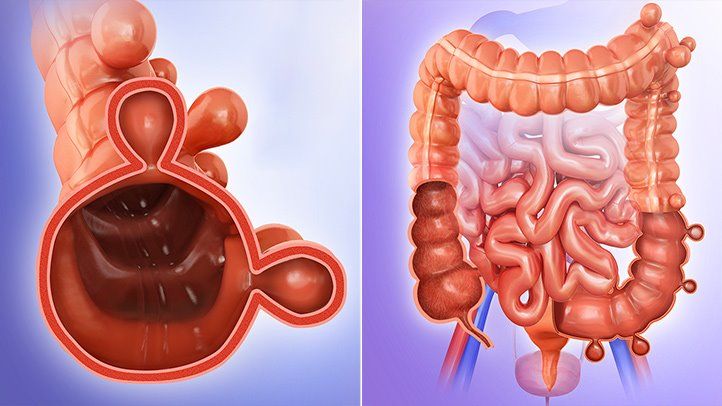
3.3. Colonoscopy
A colonoscopy involves inserting a flexible tube with a camera into the colon to directly visualize the inner lining of the colon and detect abnormalities such as diverticula, inflammation, or bleeding. However, colonoscopy is typically not used during the acute phase of diverticulitis because the procedure could potentially worsen the inflammation or cause perforation in an already compromised colon.
Colonoscopy is generally performed once the acute symptoms have subsided (in cases of non-complicated diverticulitis) to:
- Rule out other potential causes of symptoms, such as colorectal cancer or inflammatory bowel disease.
- Identify diverticula in the colon.
- Evaluate the extent of the diverticular disease and check for potential complications or other issues.
3.4. Barium Enema
A barium enema is an X-ray test in which a contrast dye (barium) is introduced into the colon through the rectum. This allows for better visualization of the colon and can help detect diverticula. However, barium enemas are rarely used to diagnose diverticulitis today due to the risk of causing perforation in patients with active inflammation.
Barium enema was once more commonly used to diagnose diverticulosis (the presence of diverticula), but because it may increase the risk of complications in acute diverticulitis, it is not routinely used in the diagnosis of sigmoid diverticulitis.
3.5. Laboratory Tests
In addition to imaging tests, several laboratory tests can help support the diagnosis of sigmoid diverticulitis:
- Complete Blood Count (CBC): A CBC may show elevated white blood cell (WBC) count, indicating an infection or inflammation. A high WBC count is commonly seen in cases of diverticulitis, especially when complications such as abscesses are present.
- C-reactive protein (CRP): CRP is an inflammatory marker that may be elevated in diverticulitis. Higher CRP levels are associated with more severe inflammation or complications.
- Urinalysis: A urinalysis may be performed to rule out other conditions, such as a urinary tract infection, that could mimic symptoms of diverticulitis.
- Stool Tests: Although stool tests are not typically used to diagnose diverticulitis, they may be performed to rule out infections that could cause similar symptoms, such as bacterial gastroenteritis or parasitic infections.
3.6. MRI (Magnetic Resonance Imaging)
In some cases, MRI may be used to diagnose sigmoid diverticulitis, especially when radiation exposure from CT scans is a concern (such as in pregnant women). MRI is less commonly used but can provide detailed images of the colon and surrounding tissues, helping to evaluate the severity of the inflammation and complications.
However, MRI is not typically the first choice for diagnosing diverticulitis, as CT scans are more widely available and faster, making them the preferred option in most cases.
4. Differential Diagnosis
Because the symptoms of sigmoid diverticulitis can overlap with other gastrointestinal conditions, a proper differential diagnosis is important. Healthcare providers must rule out conditions such as:
- Colorectal Cancer: Colon cancer can cause similar symptoms, such as abdominal pain, changes in bowel habits, and bleeding. Colonoscopy is useful for ruling out cancer.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease or ulcerative colitis can cause abdominal pain and diarrhea. These conditions often have different features on imaging and are typically diagnosed with a combination of colonoscopy and histological examination.
- Irritable Bowel Syndrome (IBS): IBS shares symptoms with diverticulitis but is a functional disorder, and does not involve inflammation or infection.
- Abdominal Abscesses: Other sources of infection in the abdomen, such as appendicitis or pelvic infections, can mimic the symptoms of diverticulitis.
Proper diagnostic testing, particularly imaging, helps distinguish sigmoid diverticulitis from these other conditions and ensures that the appropriate treatment is given.
Diagnosing sigmoid diverticulitis requires a careful combination of clinical evaluation, imaging studies, and laboratory tests. While symptoms like abdominal pain and fever are common in diverticulitis, they can also be seen in other gastrointestinal conditions, making accurate diagnosis essential. CT scans are the gold standard for confirming diverticulitis, while ultrasound, colonoscopy, and laboratory tests can further aid in assessment. Once diagnosed, prompt treatment, including antibiotics, dietary changes, or surgery, can prevent complications and improve outcomes for patients.