Key Differences Between Benign and Malignant GISTs
1.1. Tumor Behavior and Aggressiveness
The primary difference between benign and malignant GISTs lies in their biological behavior. Malignant GISTs tend to grow more rapidly, invade surrounding tissues, and have a higher likelihood of spreading to distant organs, such as the liver or peritoneum. Benign GISTs, on the other hand, grow slowly, have well-defined boundaries, and are less likely to metastasize.
- Benign GISTs: These tumors are generally small, non-invasive, and localized. They may remain asymptomatic for years and are typically removed surgically without much concern for recurrence.
- Malignant GISTs: These tumors tend to be larger, more aggressive, and invasive. They can spread to other organs and are more likely to recur after surgery. Malignant GISTs are more likely to present with symptoms such as abdominal pain, gastrointestinal bleeding, and obstruction.
1.2. Tumor Size
The size of a GIST is one of the most important indicators of its potential malignancy. Benign GISTs are usually smaller in size (often less than 5 cm) and are less likely to spread. Malignant GISTs, especially those greater than 5 cm, are more likely to show aggressive features, including a higher mitotic rate and the potential for metastasis.

- Small GISTs (less than 2 cm): These are typically benign and have a very low risk of spreading. They are often detected incidentally during imaging studies for other conditions.
- Large GISTs (greater than 5 cm): Tumors of this size are more likely to be malignant. Larger tumors have a higher mitotic rate, more invasive growth patterns, and a greater chance of metastasizing.
1.3. Mitotic Rate
The mitotic rate refers to how quickly the tumor cells are dividing. A higher mitotic rate is associated with a higher potential for malignancy. Benign GISTs tend to have a low mitotic rate, meaning that their cells are dividing slowly. In contrast, malignant GISTs have a high mitotic rate, which leads to rapid tumor growth and a higher likelihood of spreading to other parts of the body.
- Benign GISTs: Typically have a low mitotic rate (less than 5 mitoses per 50 high-power fields), indicating slower cell division and a lower risk of metastasis.
- Malignant GISTs: These tumors often show a high mitotic rate (greater than 5 mitoses per 50 high-power fields), suggesting that they are dividing more rapidly and have a higher potential for aggression.
1.4. Necrosis and Tumor Invasion
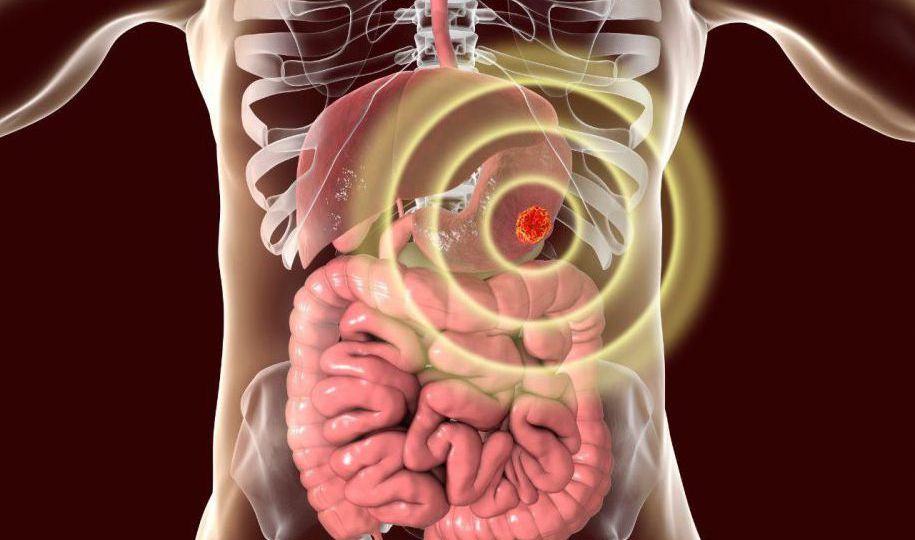
Necrosis refers to the death of tumor cells, which often occurs when the tumor grows too quickly and outgrows its blood supply. The presence of necrosis in a GIST is typically associated with more aggressive behavior and an increased risk of metastasis. Benign GISTs usually do not exhibit significant necrosis, while malignant GISTs often show substantial areas of necrosis within the tumor mass.
- Benign GISTs: These tumors tend to have minimal or no necrosis and usually do not invade surrounding tissues.
- Malignant GISTs: Malignant tumors often exhibit significant necrosis and can invade surrounding organs, blood vessels, and lymph nodes.
1.5. Genetic Mutations (KIT and PDGFRA)
Genetic mutations play a crucial role in determining the behavior of GISTs. The most common mutations found in GISTs are in the KIT gene and PDGFRA gene. While both benign and malignant GISTs can have these mutations, the presence of specific mutations can influence tumor behavior.
- KIT mutations: These are the most common mutations in GISTs and are found in approximately 70-80% of cases. Tumors with KIT mutations are more likely to respond to targeted therapies like imatinib (Gleevec), and they tend to have a more favorable prognosis, especially if the tumor is small and low-grade.
- PDGFRA mutations: These mutations are found in about 5-10% of GISTs and can be associated with both benign and malignant behavior, though they tend to occur in more indolent tumors. In general, GISTs with PDGFRA mutations have a more favorable prognosis than those with KIT mutations, particularly when the tumor is small.
Molecular testing for these genetic mutations is an essential part of diagnosing GISTs and determining the potential for malignancy.
1.6. Risk Stratification Systems
To help determine whether a GIST is benign or malignant, healthcare providers use risk stratification systems that combine tumor size, mitotic rate, and other clinical factors. The most widely used system is the Fletcher Risk Classification, which categorizes GISTs into three main groups based on their risk of recurrence and metastasis:
- Low-risk GISTs: Small tumors with a low mitotic rate and no evidence of necrosis. These tumors are generally considered benign and have a low likelihood of spreading or recurring.
- Intermediate-risk GISTs: Tumors that are larger, have a moderate mitotic rate, or show evidence of limited necrosis. These GISTs have a higher potential for recurrence and metastasis.
- High-risk GISTs: Large tumors with a high mitotic rate, significant necrosis, and a higher chance of metastasis. These tumors are more likely to recur and spread to other organs, making aggressive treatment necessary.
By assessing these factors, doctors can estimate the likelihood of malignancy and determine the best course of action for treatment and monitoring.
2. Diagnostic Approaches for Benign vs. Malignant GIST
The diagnostic process for GIST involves several key tests that help differentiate benign from malignant forms of the tumor:

2.1. Imaging Studies
Imaging tests like CT scans, MRIs, and ultrasounds are essential for detecting GISTs and evaluating their size, location, and spread. Larger GISTs with irregular borders or areas of necrosis are more likely to be malignant. These imaging tests can also help assess the presence of metastasis, which is more common in malignant tumors.
2.2. Biopsy and Histopathology
A biopsy is often performed to obtain tissue samples from the tumor for microscopic examination. Pathologists assess the tumor’s mitotic rate, necrosis, and cellular characteristics to determine whether the GIST is benign or malignant. Benign GISTs usually have well-defined borders and a low mitotic rate, while malignant GISTs show more invasive growth, necrosis, and rapid cell division.
3.3. Molecular Testing
Genetic testing, including PCR and sequencing, is essential for identifying mutations in the KIT and PDGFRA genes. These mutations are present in most GISTs and can provide information about the tumor’s behavior. Malignant GISTs tend to have more aggressive mutations, while benign GISTs often have less complex genetic profiles.
3. Treatment Approaches for Benign and Malignant GIST
The treatment for GIST largely depends on whether the tumor is benign or malignant. Surgical removal is the primary treatment for both types, but the management of malignant GISTs may also involve additional therapies.
3.1. Surgery
- Benign GISTs: These tumors are typically small and localized, making them easier to remove surgically with a lower risk of recurrence. Surgical removal is often curative.
- Malignant GISTs: These tumors are larger and more invasive, often requiring more extensive surgical intervention. In some cases, adjuvant therapies such as targeted therapy or chemotherapy may be used to reduce the risk of recurrence.
3.2. Targeted Therapy
- Imatinib (Gleevec) is the standard treatment for GISTs that express KIT mutations. This drug targets the mutated KIT protein and helps prevent tumor growth. Imatinib is most effective in malignant GISTs and is often used after surgery to prevent recurrence or metastasis.
3.3. Chemotherapy and Radiation Therapy
- While chemotherapy and radiation are generally less effective for GISTs compared to other cancers, they may be used for malignant GISTs that are resistant to targeted therapy or in cases where surgical resection is not feasible.
The distinction between benign and malignant GISTs is vital for determining the appropriate treatment and assessing the prognosis. While benign GISTs are usually small, slow-growing, and localized, malignant GISTs tend to be larger, more aggressive, and capable of spreading to other parts of the body. Understanding these differences allows healthcare providers to develop individualized treatment plans, including surgery, targeted therapy, and regular monitoring, to ensure the best possible outcomes for patients.
Advances in molecular testing, imaging, and risk stratification systems have improved our ability to differentiate between benign and malignant GISTs, providing patients with more effective treatment options and a better chance of long-term survival.