Introduction
The small intestine is a crucial part of our digestive system, responsible for absorbing most of the nutrients from the food we eat. When this part of the body is compromised due to dysfunction or disease, a condition known as Small Intestine Syndrome (SIS) can develop. Small Intestine Syndrome is an umbrella term that encompasses several gastrointestinal issues related to the malfunction of the small intestine, affecting the body’s ability to absorb nutrients properly. This condition can lead to a variety of symptoms that can range from mild discomfort to severe, chronic illness.
In this article, we will explore the various aspects of Small Intestine Syndrome: its causes, symptoms, diagnostic methods, treatment options, and how to manage the condition for long-term health. Understanding this syndrome is essential for anyone experiencing digestive issues or seeking to learn more about how this vital organ functions.
Section 1: Understanding Small Intestine Syndrome
What is Small Intestine Syndrome (SIS)?

Small Intestine Syndrome refers to a group of disorders that interfere with the normal functioning of the small intestine. This can include a range of conditions that affect the small intestine’s ability to process food, absorb nutrients, and perform its essential roles in digestion.
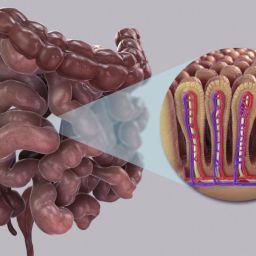
The small intestine is divided into three sections: the duodenum, jejunum, and ileum. Each section is responsible for different stages of digestion and nutrient absorption. When something disrupts the normal function of these parts, symptoms of SIS can occur.
SIS is often categorized by malabsorption, which means the body cannot effectively absorb the nutrients from food. The symptoms can vary widely depending on the severity of the condition and which part of the small intestine is affected.
Causes and Risk Factors of Small Intestine Syndrome
Several factors can contribute to the development of Small Intestine Syndrome. These include:
- Infections: Bacterial, viral, or parasitic infections in the small intestine can lead to chronic conditions like bacterial overgrowth (SIBO).
- Inflammation: Conditions like Crohn’s Disease or Celiac Disease cause inflammation in the intestines, which can lead to symptoms of SIS.
- Structural Abnormalities: Sometimes, physical obstructions or deformities in the small intestine, such as adhesions from past surgeries, can result in a reduced ability to process food.
- Malnutrition: Deficiencies in key nutrients can further exacerbate symptoms and cause long-term damage to the intestines.
- Genetic Factors: In some cases, genetic predispositions may make individuals more prone to developing certain conditions that affect the small intestine.
- Medications and Treatments: Long-term use of medications such as antibiotics or certain chemotherapy drugs can disrupt the delicate balance of gut flora and affect small intestine function.
Section 2: Symptoms of Small Intestine Syndrome
The symptoms of Small Intestine Syndrome can vary significantly depending on the specific cause and severity of the condition. In general, however, there are several common signs to watch out for.
Common Symptoms of SIS
- Abdominal Pain and Bloating: One of the hallmark symptoms of SIS is persistent abdominal pain or discomfort, often accompanied by bloating. This occurs due to inflammation or malabsorption, which causes gas and other digestive disturbances.
- Diarrhea and Constipation: Affected individuals may experience alternating bouts of diarrhea and constipation. This is a result of abnormal processing and movement of food through the small intestine.
- Nausea and Vomiting: Chronic nausea can be present, leading to a loss of appetite. In some cases, vomiting may occur, particularly if food is not being digested or absorbed properly.
- Fatigue: Due to the body’s inability to absorb nutrients effectively, people with SIS often experience chronic fatigue, which can make daily tasks difficult.
- Unintentional Weight Loss: As a result of malabsorption and poor nutrient intake, individuals may notice unexplained weight loss despite eating regularly.
Advanced Symptoms
In more severe cases of Small Intestine Syndrome, symptoms can escalate and lead to complications:

- Nutritional Deficiencies: The small intestine is responsible for absorbing nutrients like vitamins, minerals, and proteins. When it malfunctions, deficiencies in essential nutrients such as Vitamin B12, Iron, Calcium, and Vitamin D can develop, leading to anemia, bone problems, and neurological symptoms.
- Steatorrhea (Fatty Stools): This condition causes stools to appear greasy, foul-smelling, and difficult to flush, which is a sign that fats are not being properly digested or absorbed.
- Severe Dehydration: Chronic diarrhea, coupled with poor absorption, can lead to dehydration. This is especially dangerous as it affects the body’s ability to function normally.
- Appetite Changes: People with SIS may experience either a significant decrease in appetite or an increased desire to eat, as the body tries to compensate for nutrient deficiencies.
How Symptoms Can Vary
The severity of symptoms can differ based on the underlying cause of the syndrome and whether it is acute or chronic. In some cases, symptoms may flare up intermittently, while others may experience persistent, long-term discomfort. Additionally, some individuals may only experience mild symptoms, while others face more debilitating health issues.
Section 3: Diagnosing Small Intestine Syndrome
Diagnosing Small Intestine Syndrome can be a challenge, as its symptoms often overlap with those of other gastrointestinal disorders. A thorough medical evaluation is necessary for accurate diagnosis.
Medical History and Symptoms Review
The first step in diagnosis involves reviewing the patient’s medical history and symptoms. A healthcare provider will ask about the onset and frequency of symptoms, any previous gastrointestinal issues, and lifestyle factors such as diet, exercise, and stress levels.
Diagnostic Tests and Procedures
Several diagnostic tools can help in the identification of Small Intestine Syndrome:
- Blood Tests: Blood work is useful for identifying signs of infection, inflammation, or nutrient deficiencies. These tests can also help rule out other conditions like celiac disease or anemia.
- Endoscopy and Colonoscopy: These procedures allow doctors to visually inspect the small intestine and colon for abnormalities. A biopsy may also be taken during these procedures to check for signs of diseases like Crohn’s disease or infections.
- Imaging Studies: CT scans, MRIs, and ultrasounds are often used to look for any structural issues, such as blockages or adhesions, in the small intestine.
- Lactose Intolerance Test: Because lactose intolerance can cause symptoms similar to those of SIS, doctors may use this test to rule out food-related issues.
Differentiating from Other Conditions
It’s important for healthcare providers to distinguish Small Intestine Syndrome from other gastrointestinal disorders such as:
- Irritable Bowel Syndrome (IBS): A functional disorder that causes symptoms like bloating, diarrhea, and constipation, but without the malabsorption seen in SIS.
- Crohn’s Disease: An inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, including the small intestine.
- Celiac Disease: An autoimmune disorder that damages the small intestine in response to gluten.
Section 4: Treatment Options for Small Intestine Syndrome
Treatment for Small Intestine Syndrome depends on the underlying cause and severity of the condition. However, the goal is always to improve nutrient absorption, alleviate symptoms, and manage long-term health.
Dietary Management
Dietary changes are often the first step in managing Small Intestine Syndrome. Depending on the cause, some common dietary interventions may include:
- Low FODMAP Diet: This diet eliminates certain types of fermentable carbohydrates that can exacerbate symptoms.
- Gluten-Free Diet: In cases where Celiac Disease or gluten intolerance is a factor, avoiding gluten can improve small intestine function and reduce inflammation.
- Supplementation: If nutrient deficiencies are present, supplementation with vitamins and minerals, such as B12, iron, and calcium, may be necessary to restore nutritional balance.