1. Types of Rectal Surgeries
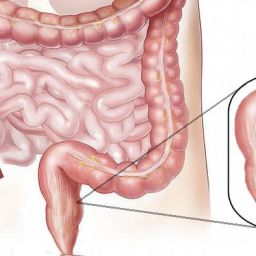
Before discussing the side effects, it’s important to understand the different types of rectal surgeries that may be performed:
- Hemorrhoidectomy: Surgical removal of hemorrhoids, often done when other treatments fail.
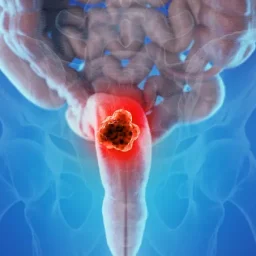
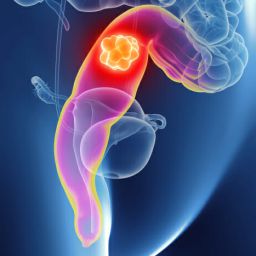
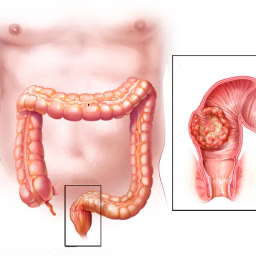
- Rectal Cancer Surgery: Includes procedures like colectomy or proctectomy to remove cancerous tissue from the rectum.
- Rectal Prolapse Surgery: Surgical correction of rectal prolapse, which occurs when the rectum protrudes from the anus.
- Anal Fissure Surgery: Removal of anal fissures or tissue repair when conservative treatments don’t work.
- Colostomy or Ileostomy: Surgical creation of an opening (stoma) in the abdomen for waste elimination when the rectum or colon needs to be bypassed.
Each type of surgery has its own set of potential side effects, which are addressed in this article.
2. Common Side Effects of Rectal Surgeries
2.1 Pain and Discomfort
Pain is a common side effect following rectal surgery. Depending on the type of surgery performed, patients may experience varying levels of discomfort. Pain is most often localized in the rectal area and can be aggravated by bowel movements, sitting, or standing for long periods. This is especially true for procedures like hemorrhoidectomy and anal fissure surgery.
- Management: Pain can usually be controlled with prescribed pain relievers, anti-inflammatory medications, and warm sitz baths. In more severe cases, stronger pain management strategies may be required.
2.2 Bleeding
Some bleeding is expected after rectal surgeries, especially those involving the removal of hemorrhoids or cancerous tissue. Minor bleeding may occur in the first few days post-surgery, but if it continues or becomes more severe, it could indicate a complication.
- Management: It’s important for patients to monitor the amount of bleeding and contact a healthcare provider if bleeding is heavy, or if it persists for more than a few days after surgery. In some cases, cauterization or other medical interventions may be required to stop the bleeding.
2.3 Infection
Infections are a risk with any surgery, including rectal surgeries. The rectal area is highly susceptible to bacterial infections due to its proximity to fecal matter, making wound care essential post-surgery.
- Signs of Infection: Redness, swelling, increased pain, pus or discharge from the surgical site, fever, or chills.
- Management: Good hygiene practices, such as keeping the area clean and dry, as well as following prescribed antibiotics, can help reduce the risk of infection. If infection is suspected, medical attention should be sought immediately.
3. Long-Term Side Effects
3.1 Incontinence
Post-surgical incontinence, or difficulty controlling bowel movements, can be a long-term side effect of certain rectal surgeries, particularly those involving the removal of part of the rectum or anal sphincter muscles. Patients may experience leakage or an urgent need to pass stool unexpectedly.
- Risk Factors: Incontinence is more likely after surgeries for rectal cancer or procedures that involve sphincter muscle repair or removal.
- Management: Pelvic floor exercises (Kegel exercises), dietary changes, and possibly physical therapy can help strengthen the muscles and manage incontinence. In some cases, further surgical intervention may be necessary.
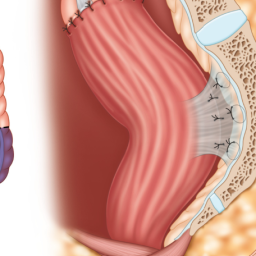
3.2 Scarring and Stenosis
Scarring is a natural part of the healing process, but excessive scarring can lead to stenosis (narrowing of the anal or rectal canal). This can make bowel movements difficult, painful, and sometimes obstructed.
- Management: Stenosis may require additional surgical procedures to widen the anal or rectal passage, or the use of dilation techniques to stretch the area.
4. Complications Related to Specific Surgeries
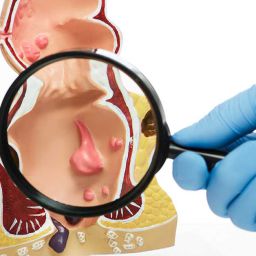
4.1 Hemorrhoidectomy Complications
Hemorrhoidectomy is one of the most common rectal surgeries, but it comes with a range of potential complications, including:
- Chronic Pain: Some patients experience pain that persists for weeks after the surgery.
- Recurrence of Hemorrhoids: In some cases, hemorrhoids can return after surgery, especially if proper post-operative care and lifestyle changes are not maintained.
- Fecal Impaction: Difficulty passing stool or constipation can occur after the procedure, leading to discomfort and the potential for further complications.
4.2 Rectal Cancer Surgery Complications
Rectal cancer surgery, depending on the extent of the disease, may involve partial or complete removal of the rectum. Potential complications include:
- Anastomotic Leak: After a colorectal resection, where parts of the intestines or rectum are reconnected, leaks can occur at the surgical site, leading to peritonitis (infection of the abdominal cavity).
- Stoma Complications: If a colostomy or ileostomy is performed, the patient may experience issues with the stoma, such as skin irritation, blockage, or leakage.
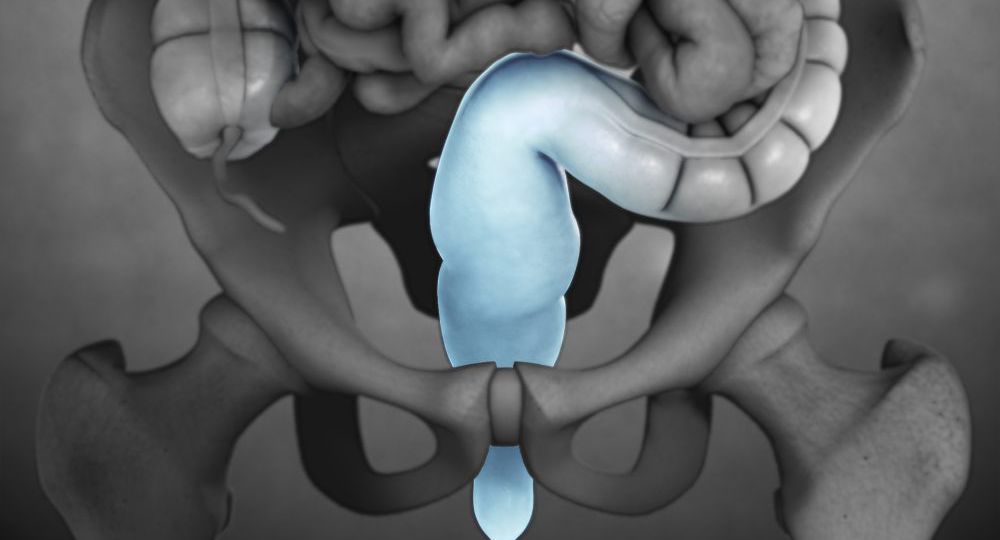
4.3 Rectal Prolapse Surgery Complications
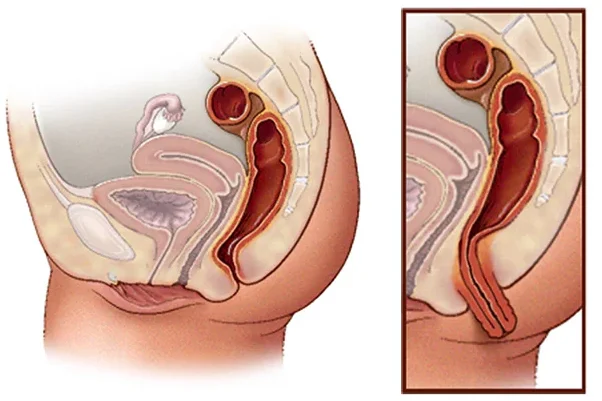
Surgical correction of rectal prolapse involves repositioning the rectum into its normal location, which carries risks like:
- Infection at the Surgical Site
- Continued Prolapse: In rare cases, the prolapse may recur after surgery.
- Urinary Issues: Some patients experience urinary retention or incontinence after rectal prolapse surgery due to the proximity of the surgery to the bladder and urinary tract.
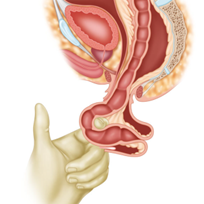
4.4 Colostomy or Ileostomy Complications
For patients who undergo a colostomy or ileostomy, complications can include:
- Stoma Rejection: The stoma site may become irritated or infected, leading to pain or difficulty managing the stoma.
- Blockage or Hernia: The bowel can become obstructed or the stoma may protrude abnormally.
- Skin Problems: Leakage or improper fitting of the colostomy bag can lead to skin irritation and discomfort.
5. Psychological Effects of Rectal Surgery
5.1 Anxiety and Depression
The psychological impact of rectal surgery should not be underestimated. Patients may experience anxiety, depression, or emotional distress related to their surgery, especially if it involves lifestyle changes, such as the use of a colostomy bag or incontinence.
- Support: Psychological counseling, support groups, or speaking with a healthcare provider about these issues can help patients cope with the emotional aftermath of surgery.
6. How to Minimize the Risk of Side Effects
6.1 Follow Post-Operative Care Instructions Following all instructions provided by the surgeon or healthcare provider is crucial for minimizing the risk of complications and side effects. This includes taking prescribed medications, attending follow-up appointments, and maintaining good hygiene.
6.2 Maintain a Healthy Diet and Lifestyle A healthy diet that includes fiber, hydration, and regular exercise can aid in recovery and prevent constipation, which can complicate rectal surgeries.
6.3 Use Pain Management Strategies Adhering to pain management protocols and using pain medications as prescribed can help manage post-surgical discomfort and prevent complications related to improper healing.
6.4 Seek Prompt Medical Attention If any unusual symptoms, such as severe pain, heavy bleeding, or signs of infection, occur after surgery, it is essential to seek medical attention immediately to prevent complications from worsening.
7. When to See a Doctor
Patients should seek medical attention if they experience:
- Severe or worsening pain that is not managed by prescribed medications.
- Heavy bleeding or persistent blood in the stool after surgery.
- Signs of infection, such as fever, redness, or discharge.
- Difficulty with bowel movements or signs of incontinence that are not improving with conservative measures.
Rectal surgeries, while often necessary for treating a variety of medical conditions, come with potential side effects that require careful management. By understanding these potential risks and complications, patients can take proactive steps to minimize their impact. Following post-operative care guidelines, seeking timely medical advice, and adopting a healthy lifestyle can significantly improve recovery outcomes and prevent long-term complications.