
What is the Spleen’s Role in the Immune System?
Before understanding the implications of splenectomy, it is essential to grasp the vital functions of the spleen:
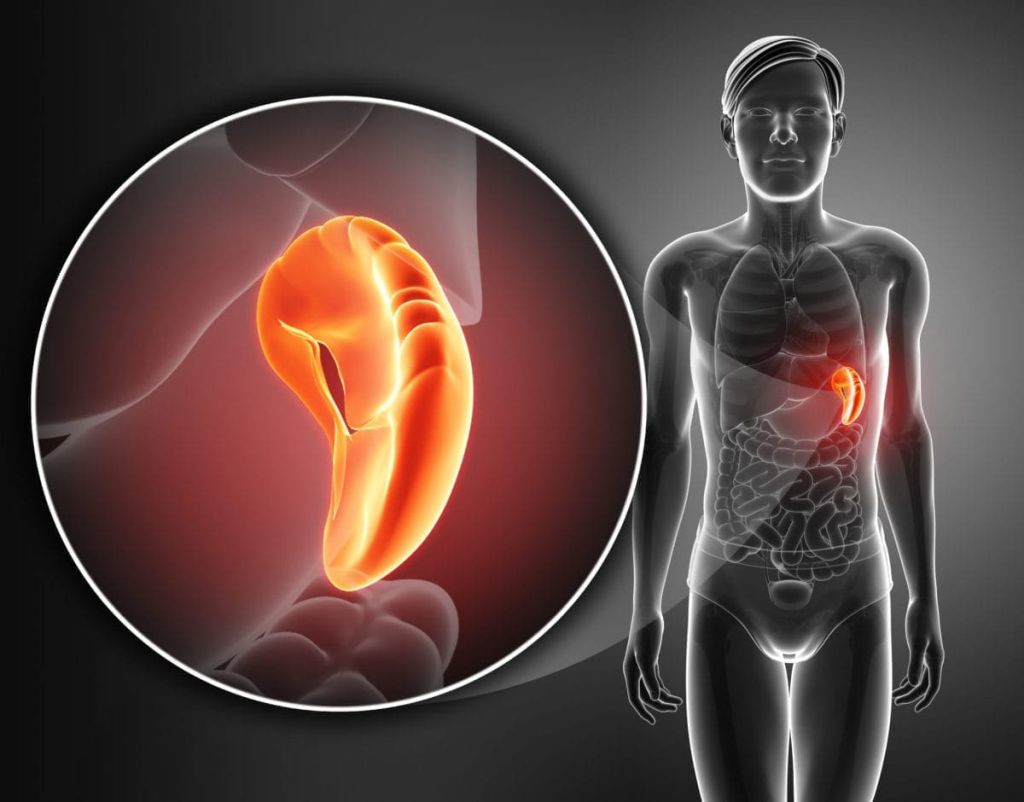
- Filtration of Blood: The spleen filters the blood, removing old or damaged red blood cells and platelets. It also helps to recycle iron.
- Immune Function: The spleen plays a major role in the immune system by filtering out bacteria, viruses, and other pathogens from the bloodstream. It houses white blood cells (such as macrophages and lymphocytes) that help fight infection.
- Storage of Blood Cells: The spleen acts as a storage site for blood cells, particularly platelets and red blood cells, which can be released into the bloodstream when necessary.
In essence, the spleen contributes significantly to maintaining the body’s defense system and balancing blood components. Therefore, its removal impacts the body’s ability to defend against infections, especially those that the spleen typically helps to neutralize.
Why is Infection Risk Increased After Splenectomy?
The spleen plays a central role in immune surveillance and response, especially against encapsulated bacteria. These are bacteria that have a protective outer coating, or capsule, which helps them evade the immune system. After a splenectomy, the body’s ability to effectively identify and eliminate these bacteria is compromised, increasing the susceptibility to severe infections. Several factors contribute to this heightened risk:
- Reduced Immune Response to Encapsulated Bacteria: The spleen is responsible for recognizing and clearing bacteria with a protective capsule. Without a spleen, the immune system’s response to these types of bacteria is less efficient.
- Decreased Phagocytic Activity: The spleen contains specialized white blood cells known as macrophages, which engulf and destroy pathogens. When the spleen is removed, the remaining organs (such as the liver and bone marrow) take over these tasks, but they are less effective, particularly in the early stages of infection.
- Absence of Antibody Production: The spleen produces antibodies in response to infections. Without the spleen, the body’s ability to produce specific antibodies on demand is delayed, which can increase the likelihood of infections becoming severe before the immune system catches up.
Common Infections After Splenectomy
While splenectomy increases the risk of infection overall, there are certain bacterial infections that are more common in post-splenectomy patients:
- Pneumococcal Infections: Caused by Streptococcus pneumoniae, these infections can lead to pneumonia, meningitis, or sepsis. They are considered the most significant risk for patients who have undergone splenectomy.
- Meningococcal Infections: Neisseria meningitidis is the causative agent of meningitis and can be particularly dangerous in post-splenectomy patients, leading to rapid sepsis and death if untreated.
- Haemophilus Influenzae Infections: This bacterium can cause severe respiratory and bloodstream infections, particularly in patients without a spleen.
- Sepsis: Without the spleen’s role in filtering pathogens, infections can rapidly progress to sepsis, a life-threatening condition that can affect multiple organ systems.
- Other Infections: Although rarer, patients who have had their spleens removed may also be at risk for infections caused by Escherichia coli, Salmonella, and other bacteria.
When is the Risk of Infection Highest?
Patients who have undergone splenectomy are at a lifelong risk of infections. However, certain factors can increase the risk during the first few months and years following the surgery:
- Immediate Post-Surgical Period: The first few weeks after surgery are critical. During this period, the immune system is in a state of recovery, and the risk of infection is higher.
- Pre-existing Health Conditions: Patients with underlying health conditions such as diabetes, liver disease, or immunodeficiencies are at even greater risk of infection after splenectomy.
- Delayed Vaccination: Delayed or incomplete vaccination schedules increase the risk of bacterial infections. Vaccination is essential before and after surgery to protect against pneumococcal, meningococcal, and Haemophilus influenzae infections.
- Age: Older patients may have a weaker immune response overall, which can increase susceptibility to infections post-splenectomy.
Prevention Strategies to Minimize Infection Risk
While the risk of infection is inevitable after splenectomy, various preventive measures can significantly reduce this risk:

- Vaccination: Pre-surgery vaccination against pneumococcal, meningococcal, and Haemophilus influenzae infections is critical. Patients should receive vaccines at least two weeks before the splenectomy procedure, or as soon as possible afterward. Booster shots should also be taken periodically.
- Antibiotic Prophylaxis: In some cases, doctors may recommend daily antibiotics (such as penicillin) for a period after the surgery, especially for young children or those at higher risk of infection. Patients should also carry an antibiotic regimen when traveling.
- Education on Signs of Infection: Educating patients on the early signs of infection, such as fever, chills, and unusual pain, can help in the prompt identification and treatment of infections. Immediate medical attention is crucial for avoiding severe complications.
- Regular Health Monitoring: Ongoing health check-ups, including blood tests and screening for infections, are necessary for splenectomy patients. Healthcare providers will monitor the patient’s immune function over time to ensure optimal protection.
- Avoiding Risky Environments: After splenectomy, patients should take extra precautions when traveling to areas with high infection rates or when exposed to certain environmental risks, such as crowd settings or unsanitary conditions.
- Long-Term Antibiotic Prophylaxis for High-Risk Patients: Some individuals may need long-term, low-dose antibiotics to prevent bacterial infections, particularly if they are at high risk due to other health conditions.
- Post-Splenectomy Care Plan: Healthcare providers will create an individualized care plan for post-splenectomy patients, which includes vaccination schedules, regular check-ups, and guidelines for preventing infections
A splenectomy is an important and sometimes life-saving procedure, but it comes with a heightened risk of infection due to the loss of an essential immune function. While the risk of infection can be lifelong, adherence to preventive measures such as vaccination, antibiotic prophylaxis, and patient education can significantly reduce the chances of post-splenectomy infections. Early diagnosis and treatment of infections are critical for minimizing complications and improving patient outcomes. By maintaining regular follow-ups and monitoring the immune system’s function, patients who have had their spleen removed can lead healthy, fulfilling lives with reduced risk.
