
Understanding Thyroid Cancer
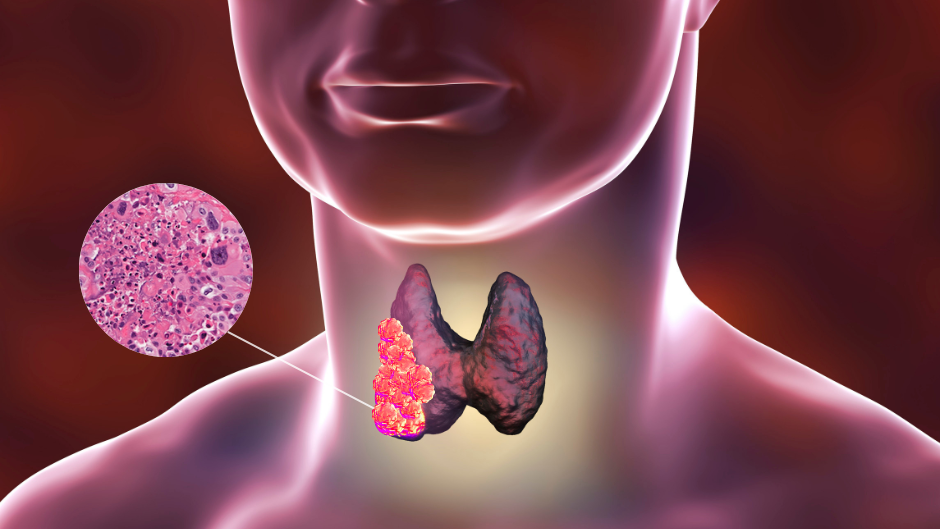
Thyroid cancer is a malignancy that originates in the thyroid gland, and it can manifest in several forms, with papillary thyroid cancer being the most common type. Thyroid cancer during pregnancy is rare, with studies suggesting that it occurs in about 1 in 100,000 pregnancies. Despite its rarity, thyroid cancer is significant because it can interfere with the delicate balance required during pregnancy.
There are four primary types of thyroid cancer:

- Papillary Thyroid Cancer (PTC): The most common type, accounting for about 80% of cases.
- Follicular Thyroid Cancer (FTC): The second most common type, usually less aggressive than papillary cancer.
- Medullary Thyroid Cancer (MTC): A rare type that originates from the C cells of the thyroid.
- Anaplastic Thyroid Cancer (ATC): An aggressive and rare form of thyroid cancer, known for poor prognosis.
Pregnancy itself doesn’t cause thyroid cancer, but certain hormonal changes during pregnancy can influence the growth of thyroid cancer cells, particularly in the early stages of pregnancy. As a result, proper diagnosis and management during pregnancy are essential to avoid complications for both mother and fetus.
Diagnosis of Thyroid Cancer During Pregnancy
The symptoms of thyroid cancer can overlap with common pregnancy-related changes, making early diagnosis challenging. Typical symptoms may include:
- A visible or palpable lump in the neck
- Difficulty swallowing or breathing
- Unexplained weight loss
- Hoarseness or voice changes
Given the overlap of these symptoms with normal pregnancy changes, it is important for pregnant women who notice any abnormalities in their neck area to consult with a healthcare provider. If thyroid cancer is suspected, diagnostic procedures typically involve:
- Physical Examination: A thorough examination to detect any lumps or unusual changes in the neck.
- Ultrasound: Non-invasive imaging is a preferred method to assess the thyroid and identify suspicious nodules.
- Fine-Needle Aspiration Biopsy (FNA): A biopsy of the thyroid nodule may be performed to determine if cancer cells are present. However, this test is usually avoided during the first trimester unless absolutely necessary.
- Blood Tests: Thyroid function tests (such as TSH, T3, and T4 levels) can help determine whether the thyroid is functioning properly.
Pregnant women should be monitored carefully, and if thyroid cancer is diagnosed, management strategies must be tailored to both the stage of the cancer and the pregnancy trimester.
Challenges of Treating Thyroid Cancer During Pregnancy
Treating thyroid cancer during pregnancy poses a series of challenges due to the potential risks to the fetus. The treatment for thyroid cancer typically involves a combination of surgery, radioactive iodine therapy, and thyroid hormone therapy. However, many of these treatments may not be safe or appropriate during pregnancy.
1. Surgery
Surgical treatment for thyroid cancer generally involves a thyroidectomy, which may be partial or complete, depending on the type and extent of the cancer. While surgery is often the first-line treatment for thyroid cancer, its timing during pregnancy must be carefully considered:
- First Trimester: Surgery is often postponed during the first trimester of pregnancy because of the increased risk of miscarriage and the effects of anesthesia on fetal development. However, if the cancer is aggressive or the tumor is rapidly growing, surgery may be necessary.
- Second and Third Trimester: Surgery can generally be performed in the second or third trimester with minimal risks to the fetus, but careful monitoring is essential.
2. Radioactive Iodine Therapy (RAI)
Radioactive iodine therapy is an important treatment for thyroid cancer, particularly for papillary and follicular thyroid cancers. However, RAI poses significant risks to the developing fetus, especially during the first trimester. The radiation can cause fetal harm, leading to birth defects, miscarriage, or developmental delays. Therefore, RAI treatment is typically postponed until after delivery, unless the cancer is aggressive and cannot wait.
3. Thyroid Hormone Therapy
Thyroid hormone replacement therapy (levothyroxine) is commonly used after surgery to ensure that the thyroid hormone levels remain stable. During pregnancy, this therapy is safe and is actually important for maintaining a healthy pregnancy, as thyroid hormones are essential for fetal brain development. Monitoring thyroid hormone levels throughout the pregnancy is crucial to ensure that both the mother and fetus receive the proper amount of thyroid hormone.
Methods to Minimize Risks for Mother and Baby
Given the potential risks of thyroid cancer treatment during pregnancy, a variety of strategies can be employed to minimize these risks and optimize outcomes for both mother and baby.

1. Timing of Treatment
One of the most important considerations is the timing of treatment. Many medical professionals recommend delaying surgery until the second trimester, which is often the safest time for both the mother and fetus. The risks associated with anesthesia and potential miscarriage are lower in the second trimester, making it an optimal time for surgery.
If surgery is needed during the first trimester, it should be performed with great caution and after careful discussion with a multidisciplinary team of specialists. In cases where immediate surgery is not necessary, close monitoring of the tumor and thyroid function may be employed until it is safe to proceed with treatment.
2. Minimizing Radiation Exposure
Because of the risks of radiation to the fetus, radioactive iodine treatment is generally avoided during pregnancy. If RAI therapy is deemed necessary after delivery, the mother should avoid breastfeeding for a period of time to prevent radiation exposure to the infant.
In cases where radiation therapy cannot be postponed, the healthcare provider must take steps to limit the exposure, including isolating the patient after treatment and closely monitoring both the mother and baby.
3. Thyroid Hormone Replacement
Pregnant women with thyroid cancer who have had thyroid surgery will likely need thyroid hormone replacement therapy. Ensuring that thyroid hormone levels are within the appropriate range is essential for maintaining the health of the mother and supporting fetal development. Adequate thyroid hormone levels are critical for normal brain development in the fetus, especially during the early stages of pregnancy.
Doctors will adjust the dose of levothyroxine during pregnancy to ensure optimal thyroid function for both the mother and baby. Regular monitoring of thyroid function is important to adjust dosages and maintain a stable hormonal balance.
4. Psychological Support and Counseling
Being diagnosed with thyroid cancer during pregnancy can be overwhelming for the expectant mother. The emotional toll of managing a cancer diagnosis while preparing for childbirth can affect mental health. Offering psychological support, counseling, and a supportive network can help alleviate stress and anxiety, promoting better overall health outcomes for both the mother and baby.
5. Postpartum Monitoring and Care
After childbirth, mothers who have had thyroid cancer may require additional monitoring and follow-up care. The postpartum period can sometimes exacerbate thyroid issues, and healthcare providers should continue to monitor thyroid function and ensure that cancer treatment is followed up appropriately.
Thyroid cancer treatment during pregnancy requires a delicate balance between effective cancer management and the health and safety of both the mother and the fetus. With proper medical management, a multidisciplinary team of specialists, and careful consideration of the timing of treatments, many women with thyroid cancer can experience successful outcomes during pregnancy.
By delaying certain treatments such as radioactive iodine therapy until after delivery, avoiding unnecessary surgical procedures during the first trimester, and ensuring proper thyroid hormone levels, the risks associated with thyroid cancer during pregnancy can be minimized. However, each case is unique, and close monitoring is essential to ensure the best possible outcomes for both the mother and the baby.
For pregnant women diagnosed with thyroid cancer, understanding the risks, options, and available treatments is critical to making informed decisions and navigating this challenging time with confidence and care.
